What is a Variant?: Understanding the Virus Game-Changer
Viruses are different from one another in many ways, including how well they spread and which parts of the body they attack. One thing most viruses have in common, though, is that they have resourceful ways to survive our efforts to kill them. As they infect and reproduce in living things, their genetic makeup changes. Some changes, or mutations, can cause a virus to be more contagious or make the host more sick. This survival mechanism helps many of these viruses with genetic variations, known as variants, to stick around in a population longer.1
The ongoing genetic change in viruses is one of the main reasons we get flu shots once a year and one of the factors that makes eradicating COVID-19 a challenge. Infectious disease expert Alejandro Cané, MD, Pfizer’s Scientific and Medical Affairs Lead of Vaccines, says it’s a natural process.
“As they infect humans and animals, viruses are constantly changing all the time,” says Dr. Cané. “And any single change they make in their genomic sequence can create what we call a mutation. These mutations can lead to a variant of the virus which can, in turn, behave differently than the original virus.”
How Do Variants Happen?
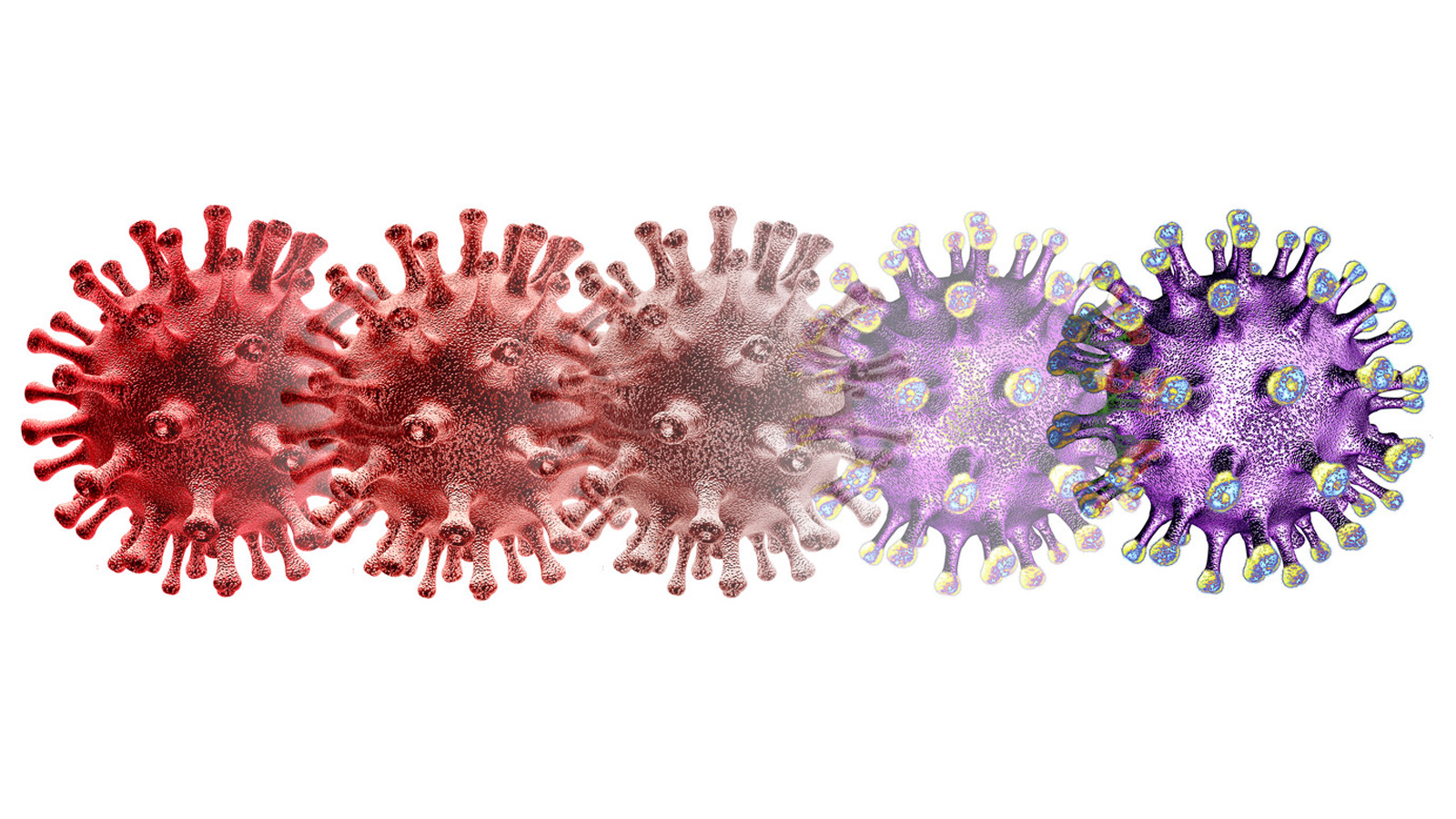
Variants occur when viruses reproduce and infect new people and animals. Think of it like a photocopy: When you copy a document, there’s always a chance that errors happen—like when text gets cut off or becomes too faded to read. The more you copy the copies, the more significant these errors become.
Viruses change similarly.
“When viruses infect an animal or human cell, they use that animal or human’s genetic code to reproduce and they multiply that same process millions of times,” Dr. Cané says. “But at the same time, viruses have to escape from the hosts’ immune system, which can kill the virus. So they’re able to produce small changes that allow them to survive in that particular animal or human.”
Some viruses are bad at adapting and die off quickly. But others are good. Really good. And the good ones create variants that help the virus survive and infect more living beings so that it can continue to spread and mutate over time.1
When Variants Become Concerning
Variants are natural, but it doesn’t mean they’re not alarming. To understand why, Dr. Cané says to imagine a virus as a tree: It begins with the trunk, eventually growing into different limbs and branches. As it reproduces, scientists can differentiate the branches from one another and may be able to create vaccines that can work against them.
Sometimes a virus can mutate so drastically and quickly that it’s considered a whole new family of viruses, known as a strain. This happened when a new H1N1 flu virus appeared, causing the 2009 swine flu pandemic. Unfortunately, the seasonal flu shot didn’t help curb the spread because it was not designed to protect people from that specific variant of the flu virus.2
The COVID-19 variants could present similar problems. As the virus that causes COVID-19 spreads, its mutations have led to new variants, such as the Delta and Omicron variants, that could potentially be shown to make the disease more deadly or more transmissible.3,4
“While COVID-19 vaccines have been shown to work pretty well against severe infection and hospitalization due to existing variants so far, a future mutation could change the virus so much that it potentially evades the vaccine,” Dr. Cané says. “This is the reason why epidemiological surveillance and real-world data collection are critical to monitor the evolution of the pandemic”
Researchers like Dr. Cané are watching variants closely to make sure the vaccines we have remain effective and that scientists can adjust the vaccines as needed to keep up with the changing virus.
“We’re always looking at how each of these variants behaves in terms of infections and deaths,” Dr. Cané says. “When a new variant is discovered, we immediately check in the lab to see how our vaccines perform against it.”
What You Can Do
If you’re worried about variants, here’s what to do: Get your recommended vaccines.
Viruses need bodies to infect before they can create new variants. But if everyone is vaccinated, it can limit that virus’s ability to mutate.1
Older generations saw this protection from polio. Once a devastating disease, polio is no longer the public health threat it once was. By immunizing people against it so the poliovirus couldn’t spread and mutate, vaccines helped us turn a corner on the U.S. polio epidemic.5
“If you have fewer people infected, you have less risk to see new viruses in the community where you live,” Dr. Cané said. “We like to see higher than 70% to 75% percent of the population vaccinated so that you limit where viruses can spread.”
Vaccines are widely available for diseases such as influenza, polio, hepatitis, and COVID-19. By following your doctor’s instructions about which shots to get and when to protect yourself and your loved ones, you CAN have a role to play in stopping not only the spread of variants but their very creation.
References:
1. Sanjuán R., Domingo-Calap P. Mechanisms of viral mutation. Cell Mol Life Sci. 2016;73(23):4433-4448. Accessed February 2, 2022. doi: 10.1007/s00018-016-2299-6.
2. Centers for Disease Control and Prevention. Effectiveness of 2008–2009 Trivalent Influenza Vaccine Against 2009 Pandemic Influenza A (H1N1) – United States, May–June 2009. MMWR. 2009; 58(44):1241-1245. Accessed February 2, 2022. https://www.cdc.gov/mmwr/pdf/wk/mm5844.pdf
3. Centers for Disease Control and Prevention. Delta Variant: What We Know About the Science. Updated August 26, 2021. Accessed February, 2, 2022. https://www.cdc.gov/coronavirus/2019-ncov/variants/delta-variant.html
4. Centers for Disease Control and Prevention. Omicron Variant: What You Need to Know. Updated February 2, 2022. Accessed February 2, 2022. https://www.cdc.gov/coronavirus/2019-ncov/variants/omicron-variant.html
5. Baicus A. History of polio vaccination. World J Virol. 2012;1(4):108-114. doi: 10.5501/wjv.v1.i4.108
![]()
