What is Sarcoidosis?: Your Questions Answered
Imagine waking up one morning and finding tender, red bumps all over your skin. Your vision is a bit blurry, so you check your eyes in the mirror. They’re red and teary. Is it allergies?
Weeks go by, but you don’t get any better. One day, you feel feverish and short of breath, and you notice that your lymph nodes are swollen.
Something is amiss. You make a doctor’s appointment, but the symptoms miraculously vanish.
The cycle repeats for years as you bounce from doctor to doctor, taking test after test, all the while feeling confused and frightened. Finally, a lung biopsy reveals a diagnosis: sarcoidosis, an illness characterized by inflammation of the organs. While you’re relieved that your condition has a name, the roller coaster ride of confusion rolls on.
Sarcoidosis: A Rare Disease
This scene describes the reality of life with sarcoidosis, a disease that medical experts estimate affects between 150,000 and 200,000 Americans,1 often between 20 and 60 years old.2 While it affects people all over the world, sarcoidosis appears to be more prominent among and people of Northern European or African descent.
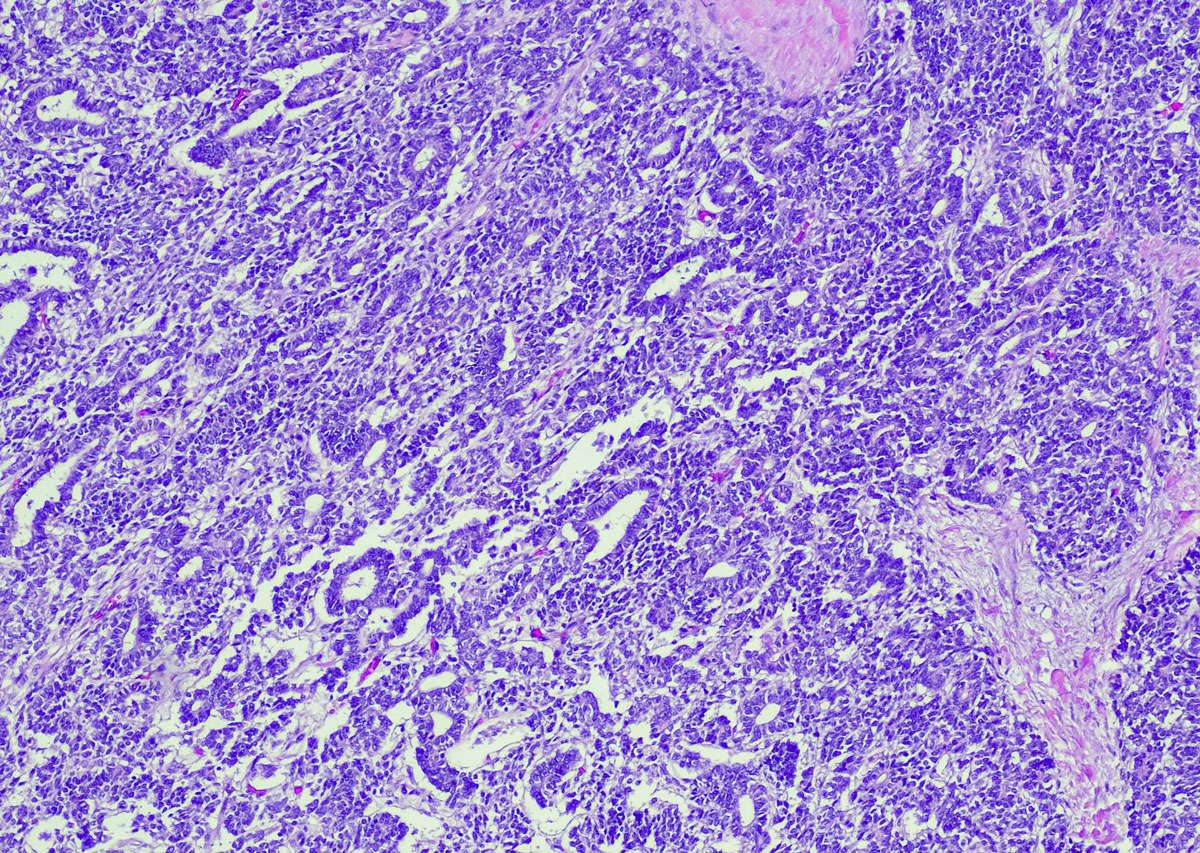
Sarcoidosis can cause inflammation in almost any organ. Typically, however, it affects the lungs. Wherever it develops, sarcoidosis causes clumps of inflamed cells, called granulomas.
Sarcoidosis Could Point to an Overactive Immune System
While research has yet to identify the precise cause, people who receive a sarcoidosis diagnosis must consider the possibility that the disease is a product of their own body attacking itself.2
Most of the time, the human immune system is an ally that defends our bodies from unwanted intrusions, such as viruses and bacteria. But for those with sarcoidosis, an over-active immune system creates trouble, attacking otherwise healthy tissue and organs.1
The disease may begin with environmental exposure. Something in the air, water, or food triggers a chain reaction of inflammation and immune responses. Eventually, healthy organs become overwhelmed by all this immune activity and suffer damage.1,2
Although this situation may sound dire, that isn’t always the case. In some patients, symptoms may resolve without treatment in a few years.3 But any old scars will remain and can still cause symptoms.3
Finally, some (5%-10%) may experience advanced sarcoidosis, which involves worsening symptoms.1 If left untreated, around 5% of people with sarcoidosis will die from the disease.4
Diagnosing Sarcoidosis Can Take Years
Navigating sarcoidosis can be frightening and confusing. For example, some people with sarcoidosis experience no symptoms. Then a chest X-ray reveals the presence or extent of the disease.. For other people, symptoms are often specific to the affected organs, such as the kidneys or heart. Other common symptoms of sarcoidosis can include fatigue, joint or muscle pain, and swollen lymph nodes.4
To diagnose sarcoidosis, physicians perform a biopsy, taking a small tissue sample from the affected organ to study under a microscope.4 Experts look for those abnormal clumps of inflammatory immune cells, known as granulomas, that typify this disease.2,3
Granulomas result from inflammation, although the causes of the inflammatory attack and granuloma build up vary.5 If left untreated, the presence of granulomas can scar tissues (fibrosis), which may cause long-term organ problems.1,3
Unfortunately, arriving at a sarcoidosis diagnosis can be a challenging process.1 Physicians must first rule out other possible diagnoses that can also be associated with granulomatous inflammation, such as tuberculosis infections or lung disease6 from beryllium or silica dust inhalation.7
Testing also adds time to the process. There is no specific test for sarcoidosis. Physicians must rely on an array of exams, including X-rays, biopsies, blood tests, and breathing tests.4
Treating Sarcoidosis
There’s no cure for sarcoidosis, yet.1 But doctors can prescribe medications to help manage symptoms.4
Many people diagnosed with less severe sarcoidosis are simply monitored without specific treatment over time.4 Most commonly, when treatment is required, a doctor might prescribe a steroid to control inflammation or a drug to suppress the overactive immune system.8,9 Doctors might also use an antimalarial to treat the skin or a drug used for rheumatoid arthritis.9,10
There’s also hope for a new prescription fusion protein that received Orphan Drug Designation from the FDA in April 2022.11 This designation is reserved for drugs that might benefit people with rare diseases, even if the market is small.12 Because new drugs require vast sums of money to develop, the federal government supports the development of promising orphan drugs.13
People with symptoms that suggest sarcoidosis should not wait to see their healthcare providers. Diagnosing and treating sarcoidosis can take time, since symptoms vary and may affect multiple organs and body parts.1,4 Be prepared to give your physician a complete history, including questions to eliminate other causes of your symptoms.
Sources
- Foundation for Sarcoidosis Research. Sarcoidosis, What is it? https://www.stopsarcoidosis.org/what-is-sarcoidosis. Accessed January 20, 2023.
- Starshinova AA, Malkova AM, Basantsova NY, et al. Sarcoidosis as an autoimmune disease. Front Immunol. 2020;10:2933.
- American Thoracic Society. Treatment of Sarcoidosis. https://www.thoracic.org/patients/patient-resources/resources/sarcoidosis-pt-2-treatment.pdf. January 20, 2023.
- Bokhari S. Zulfiqar H, Mansur A. Sarcoidosis. StatPearls. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK430687/.
- Williams, Olivia and Saira Fatima. Granuloma. StatPerals. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK554586/. Updated September 19, 2022. Accessed January 20, 2023.
- Badar F, Azfar SF, Ahmad I, Yasmeen S, Kirmani S. Diagnostic difficulties in differentiating sarcoidosis from tuberculosis. Oman Med J. 2011;26(3):210-211. ncbi.nlm.nih.gov/pmc/articles/PMC3191697. Accessed January 20, 2023.
- Graff P, Larsson J, Bryngelsson IL, Wiebert P, Vihlborg P. Sarcoidosis and silica dust exposure among men in Sweden: a case–control study. BMJ Open. 2020;10(9):e038926. https://bmjopen.bmj.com/content/10/9/e038926. Published September 3, 2020. Accessed January 20, 2023.
- Soto-Gomez N, Peters JI, Nambiar AM. Diagnosis and management of sarcoidosis. Am Fam Physician. 2016;93(10):840-848.
- Vermeer B, Veltkamp M, Vorselaars AD. Effect of hydroxychloroquine in cutaneous sarcoidosis or musculoskeletal-related pain. In: 12.03 - Sarcoidosis and Other Granulomatous ILD/DPLD. European Respiratory Society; 2022:763.
- Fang C, Zhang Q, Wang N, Jing X, Xu Z. Effectiveness and tolerability of methotrexate in pulmonary sarcoidosis: A single center real-world study. Sarcoidosis Vasculitis and Diffuse Lung Disease. 2019;36(3):217-227.
- aTyr Pharma Announces FDA Orphan Drug Designation… for Treatment of Systemic Sclerosis https://www.globenewswire.com/news-release/2022/04/13/2421843/0/en/aTyr-Pharma-Announces-FDA-Orphan-Drug-Designation-for-Efzofitimod-ATYR1923-for-Treatment-of-Systemic-Sclerosis.html. Published April 13, 2022. Accessed January 20, 2023.
- U.S. Food and Drug Administration. Orphan Drugs. https://www.fda.gov/media/83372/download. Published July 13, 2012. Accessed January 20, 2023.
- U.S. Food and Drug Administration. Designating an Orphan Product: Drugs and Biological Products. https://www.fda.gov/industry/medical-products-rare-diseases-and-conditions/designating-orphan-product-drugs-and-biological-products. Updated July 8, 2022. Accessed January 20, 2023.