New Pathways to Cachexia Treatment: Focusing on Patient Quality of Life
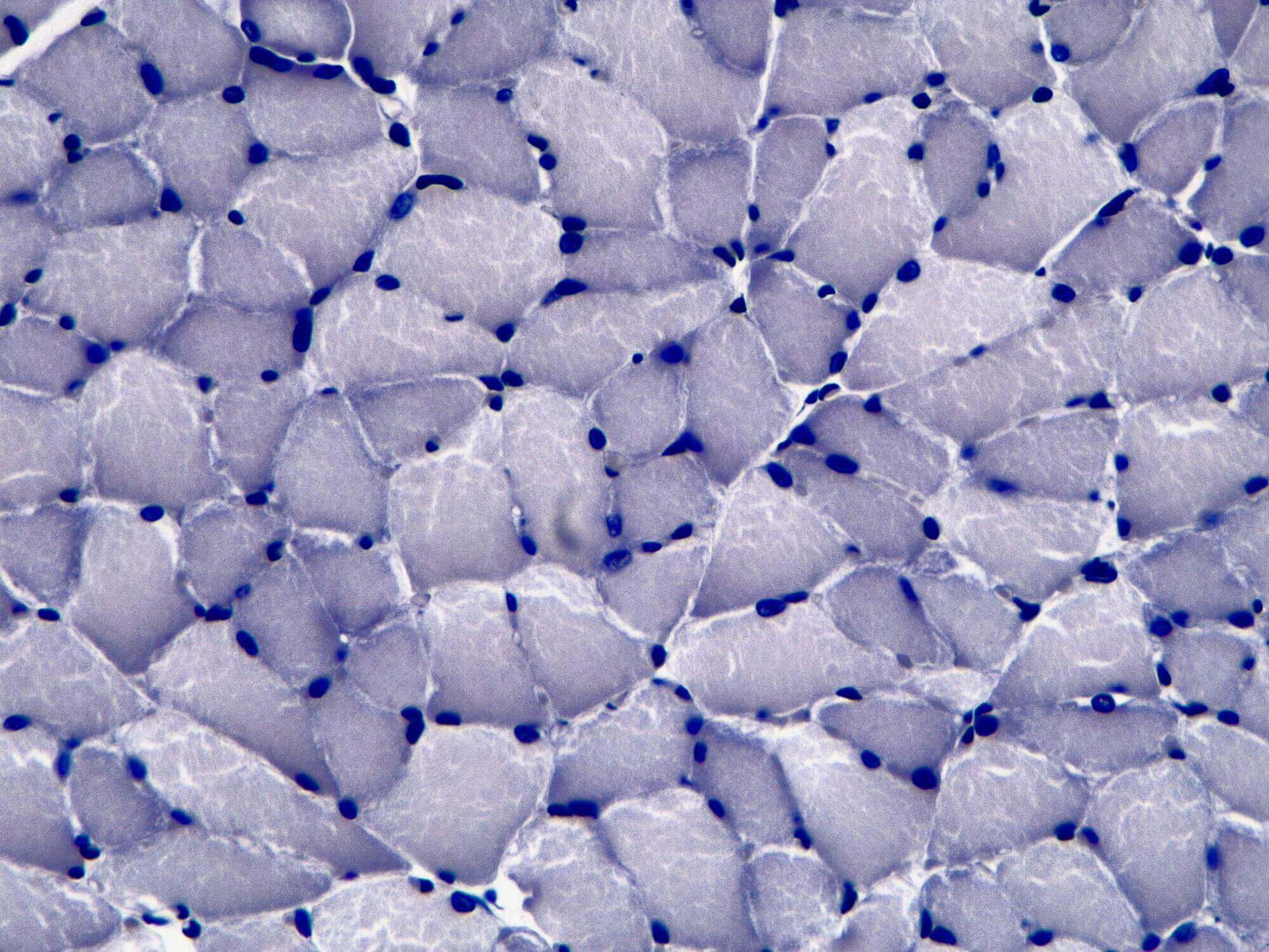
Patients living with certain underlying chronic illnesses, such as cancer, chronic obstructive pulmonary disease (COPD), congestive heart failure, and other diseases often experience a syndrome called cachexia, which can cause anorexia, unintentional weight loss, muscle wasting, loss of appetite, and/or fatigue.1, 2, 3 This wasting disorder can severely impact patients’ quality of life, and in some cases, such as cancer, hinder their ability to continue treatment for the primary illness.3
Despite an urgent need, researchers have thus far had little success addressing this multisystem disease.3 But in recent years, as scientists have gained better understanding of the biology behind the condition, they are focusing on specific metabolic and inflammatory pathways as potential treatment targets. Pfizer researchers are currently pursuing programs in several cachexia drug targets, with the goal of developing multi-modal interventions that target loss of appetite, weight loss, muscle wasting, and/or inflammation.
“Our scientific approach is to really listen to patients and to enhance our understanding of the underlying biological mechanisms driving the disorder,” says Zhidan Wu, a Senior Scientific Director based at Pfizer’s Cambridge, Mass. research site. “And we’re focusing on several key pathways that can potentially improve patients’ symptoms.”
Tackling multiple symptoms
In the past, cachexia treatment research hit roadblocks because it often focused solely on therapies to reverse muscle wasting, only one aspect of the disease. But Pfizer’s new efforts are aimed at tackling multiple symptoms at once. “We’re either using one target with a lot of horsepower or multiple targets in combination that could treat multiple aspects of the disease,” says Danna Breen, a Senior Principal Scientist, also based at Pfizer’s research site in Cambridge.
Pfizer’s flagship cachexia program focuses in on growth differentiation factor-15 (GDF-15), a cytokine, or cellular signaling protein, that is linked to appetite and energy regulation. Patients with late-stage illnesses, particularly cancer, have elevated levels of this signaling protein. It’s believed that GDF-15 interacts with receptors in the brain related to appetite control, causing loss of appetite and nausea. “It's probably one of the most powerful mechanisms that we've seen so far, at least pre-clinically, in terms of regulating appetite and weight loss in chronically ill patients,” says Wu.
Pfizer scientists are working to develop an antibody that could block GDF-15 in cachexia patients and potentially help patients restore their appetite and gain weight.
Cachexia in cancer patients
For the recent American Society of Clinical Oncology (ASCO) conference (which was held virtually this year), Pfizer scientists shared several research abstracts related to their GDF-15 pre-clinical research. One noteworthy study examined GDF-15 and its link to common side effects experienced by cancer patients undergoing platinum-based chemotherapy treatment, including loss of appetite, nausea, and vomiting. “We believe that the toxic side effects from certain chemotherapies may produce a stress response causing many different cell types to turn into GDF-15 producers,” says Breen.
Using pre-clinical models, scientists found that a GDF-15 blocking antibody could help restore appetite and weight gain. While the research is still early, scientists hope these results could translate to cancer patients, who often have to limit their chemotherapy doses due to loss of body weight. “We would enable patients to have the optimal dose for their cancer treatments, as well as mitigate some of the side effects to improve their quality of life,” says Wu.
Complementary approaches
Pfizer scientists are also pursuing separate cachexia programs to combat anorexia and weight loss, which are designed to be complementary to the GDF-15 antibody. “Novel science is emerging to increase our understanding of how these pathways interact with one another,” says Breen. “Hopefully, this will lead us to identify the most effective therapies,” she adds.
And taking a patient-centered approach, researchers can then tailor cachexia treatment combinations based on patients’ needs. “We’re really focused on improving patient quality of life,” says Breen.
