Early Detection is Key
In the fight against cancer, every screening, every result, every early detection matters. Join the fight against cancer and get screened at PfizerForAll.com/Screenings.
![]()
Bladder cancer is a type of cancer that forms in the bladder, a hollow, balloon-shaped organ located in the lower portion of the abdomen.1,2 The bladder stores urine, a liquid containing the body’s waste products, until it’s passed out of the body. 1,3 Urine travels from the kidneys to the bladder through small tubes called ureters. As urine enters the bladder, the bladder’s muscular wall stretches, allowing a buildup of urine—eventually, this muscular wall contracts, forcing urine to exit the body through a tube called the urethra.2
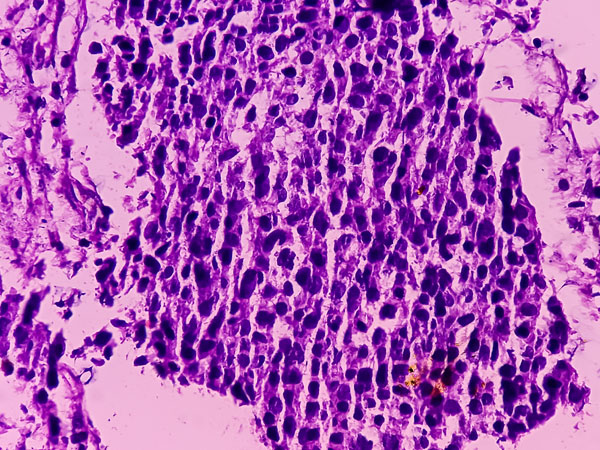
In most cases, cancer develops in the innermost lining of the bladder, known as the urothelium, or transitional epithelium. Urothelial cells also line the innermost portions of other parts of the urinary system, including part of each kidney, the ureters, and the urethra. Cancer can develop in any of these places, so a person diagnosed with bladder cancer should be thoroughly checked for tumors in these areas outside the bladder.1
Bladder cancer that begins in the urothelium may eventually spread to other layers of the bladder itself. In some cases, cancer that invades the deeper layers of the bladder eventually spreads through the bladder and into nearby or distant organs, including lymph nodes, bones, the liver, or the lungs.1
Generally, bladder cancer is more difficult to treat the farther it spreads.1 However, new tests to help diagnose bladder cancer earlier, as well as new treatments for the condition, may eventually help more people achieve more positive outcomes.4
Bladder cancer is the 10th leading cause of cancer deaths in the United States. Anyone assigned female at birth has about a 0.3 percent chance of dying from bladder cancer. Any person assigned male at birth has about a 0.8 percent chance of dying from bladder cancer.5
In 2025, the American Cancer Society predicts that doctors will diagnose almost 85,000 new cases of bladder cancer:5
It’s expected that a little over 17,000 deaths will result from the disease:5
While smoking is the main risk factor for bladder cancer, the disease also tends to occur more frequently in people assigned male at birth.5 And although anyone can develop bladder cancer, the condition is most often diagnosed in older people. It is also more likely for white people to develop bladder cancer compared to Black people.6
Among all people, bladder cancer rates have fallen since 2013 by approximately 1 percent. This is most likely due to a general decrease in the number of people who smoke. Death rates from bladder cancer have also fallen by about 1 percent, probably thanks to increased awareness of the condition, earlier detection, and access to better treatments.5
The exact cause of bladder cancer is unknown. However, scientists know that changes in a person’s DNA, which makes up a person’s genes, changes how cells normally function. These changes, known as mutations, may cause cells to grow out of control and form cancerous tumors.7
Gene mutations may be acquired or inherited, and either may result in the development of cancer. Acquired mutations happen at random over the course of a person’s life. They may result from exposure to cancer-causing chemicals, such as tobacco smoke or radiation.7
Inherited mutations, or those passed on from parents to children, aren’t thought of as a major cause of bladder cancer since the disease doesn’t usually run in families. However, a person may inherit a genetic mutation that lowers the body’s ability to break down and get rid of some types of cancer-causing chemicals. These individuals may therefore be more likely to develop cancer after exposure to things like tobacco smoke or industrial chemicals.7
A family history of bladder cancer may increase a person’s risk of developing the disease.3,6 Scientists speculate that this happens because of shared genetic mutations that make it harder for the body to break down harmful substances or shared environmental exposures.8
Although uncommon, some people do inherit genetic syndromes that increase the risk of bladder and other types of cancer. Some of these syndromes include:8
A variety of risk factors may increase a person’s likelihood of developing bladder cancer, although they do not guarantee it. While some risk factors cannot be changed, others, like whether a person smokes, can be.8
Smoking is thought to be the most important risk factor for bladder cancer.3 Research links smoking to almost half of all bladder cancer cases. Additionally, smoking may increase the risk of bladder cancer by at least three times compared to people who don’t smoke.8
All tobacco products contain carcinogens, or chemicals that may cause cancer.9 When a person smokes, these chemicals absorb into the bloodstream. Then, they’re filtered by the kidneys before collecting in the bladder in urine. The exposure of the bladder to these chemicals may damage DNA and result in the formation of cancer.6
Contact with or exposure to industrial chemicals is also linked to bladder cancer. For example, chemicals in the dye industry, such as aromatic amines like benzidine, may cause bladder cancer.8
Other industries whose workers may have an increased risk of bladder cancer due to chemical exposure include those that produce:8
Certain occupations may also be more likely to develop bladder cancer, including:8
A certain diabetes medication, called pioglitazone, may increase the risk of bladder cancer, particularly if higher doses of the medication are prescribed. Also, certain dietary supplements containing aristolochic acid could increase a person’s risk.8
In some parts of the world, water supplies contain arsenic. Although uncommon in the U.S., people in other countries could be exposed to arsenic in drinking water, thereby increasing their risk for bladder cancer.8
Some research suggests that people who drink a large volume of fluids every day are not as likely to get bladder cancer.8
Studies indicate that white people are almost two times more likely to develop bladder cancer compared to Black and Hispanic people. Also, people of Asian descent seem to be less likely to get this condition.8
The risk of bladder cancer increases with age. Most people who receive a diagnosis are over the age of 55.8
Those assigned male at birth are more likely to develop bladder cancer compared to those assigned female at birth.8
A personal history of frequent or ongoing bladder infections, kidney and bladder stones, and urinary catheters left in place for a long time have been linked to bladder cancer.8
In some parts of the world, such as Africa and the Middle East, infection with a parasitic worm known as schistosomiasis (or bilharziasis) can increase the risk of bladder cancer. This is extremely rare in the U.S.8
Any cancer that affects any part of the urothelium, or the innermost lining of the urinary tract, places an individual at higher risk of bladder cancer. This occurs even if previous urinary tract cancers have been successfully treated.8
During fetal development, a connection exists between the bladder and belly button that’s known as urachus. Normally, this connection disappears after birth. If it remains, the person is at higher risk of bladder cancer.8
Another birth defect, known as exstrophy, happens when the bladder and the abdominal wall in front of it fuse together, exposing the bladder lining to the environment outside the body. This increases a person’s risk of bladder cancer even if this condition is corrected with surgery soon after birth.8
A family history of bladder cancer increases an individual’s risk for developing bladder cancer themselves, although it is not a guarantee that cancer will occur.8
A chemotherapy medication, known as cyclophosphamide, may irritate the bladder if used over long periods of time. Bladder irritants may increase the risk of bladder cancer. Additionally, pelvic exposure to radiation may also be a risk factor.8
There is currently no guaranteed way to prevent bladder cancer. However, you can lower your risk by managing certain risk factors, like smoking. If you smoke, the best way to help prevent bladder cancer is to stop. People working in industries that expose them to harmful chemicals should also follow appropriate workplace safety practices.10
A healthy diet consisting of plenty of fruits and vegetables may also help prevent cancer, and drinking plenty of fluids throughout the day may also help. If you live in a place with arsenic in drinking water, try to limit your exposure by using alternate water sources, like bottled water.10
Bladder cancer isn’t just one single disease—there are several different types of bladder cancer a person may develop. Most bladder cancers are urothelial carcinomas (transitional cell carcinomas). This type of cancer begins in the urothelial cells that line the innermost portions of the urinary tract, including the bladder, ureters, urethra, and portions of each kidney. By far, most diagnosed cases of bladder cancer are urothelial carcinomas.1
There are several other types of bladder cancer, including but not limited to:1,2
Additionally, bladder cancer can be grouped into two categories depending on whether cancerous cells are present in the muscle layer of the bladder wall:1,2
Non-invasive bladder cancers can be further subdivided into two main subtypes:1

Bladder cancer symptoms can vary greatly from person to person—many are the same as symptoms for other medical conditions or diseases that aren’t cancer, like urinary tract infections, bladder stones, or an enlarged prostate. Blood in the urine is often the first symptom noticed. It’s possible for blood to appear and then not reappear for a period of time. In some cases, blood in the urine is only detectable using laboratory tests.11,12
Other common symptoms of bladder cancer have to do with changes in urination, such as:11,12
When bladder cancer becomes more advanced and grows or spreads beyond the bladder, symptoms may include:11,12

Complications from bladder cancer are possible and may result from cancerous cells that have spread to other tissues or organs. In some cases, bladder cancer cells travel through pelvic lymph nodes to other areas of the body, like the bones, liver, or lungs.13
Beyond the spread of bladder cancer itself, other complications from the disease may include:13
Doctors rely on several diagnostic tests to determine whether a person has bladder cancer.14 If cancer is found, treatment will likely include a combination of several therapies.
Doctors use multiple tests and examinations to accurately diagnose bladder cancer.
Many doctors begin by taking your medical history and performing a physical examination. During this exam, your doctor may perform a digital rectal examination (DRE). During this simple procedure, a doctor inserts a gloved, lubricated finger into your rectum to feel for bladder tumors. People assigned female at birth may also undergo a pelvic exam.14
Testing your urine for signs of bladder cancer can help your doctor diagnose the condition. These tests may include:14,15
Cystoscopy, a procedure performed by a urologist, is often recommended when doctors suspect bladder cancer. During the procedure, the urologist uses a long, flexible tube, called a cystoscope, to view the interior portion of the bladder. The cystoscope has a light source and a small camera to allow for better viewing.14,15
A urologist inserts the cystoscope through the urethra and into the bladder. In some cases, doctors also take samples of bladder tissue (biopsy) for further testing. Additionally, doctors may use a fluorescent dye to help identify bladder cancer cells—the dye is actively absorbed by cancerous cells, making them much easier to visualize.14,15
During this procedure, doctors remove any detected tumors from the lining of the bladder. Some bladder muscle surrounding those tumors is also usually removed. Then, those samples go to a laboratory for more testing.14
Imaging tests help doctors determine the location of the bladder cancer and whether it has spread to nearby lymph nodes or other tissues. Your doctor may suggest:14,15
A biopsy, or the collection of a tissue sample from an area of suspected cancer, helps doctors make a definitive diagnosis of bladder cancer. Often performed during a cystoscopy, the sample collected helps discover more information about the cancer, such as:14,15
Although not appropriate for everyone, genetic testing may help those with inherited genetic changes better understand their risk. This is usually recommended for people:14
Determining the bladder cancer’s stage is important for planning treatment. The stage of the cancer refers to if and how far the cancer has spread.16
Doctors most often use the American Joint Committee on Cancer’s (AJCC) TNM system to help stage cancer:16
TNM staging combines with stage grouping to determine an overall cancer stage. Stage grouping indicates just how far bladder cancer has spread, with stage 0 (non-invasive) as the earliest stage and stage IV as the most advanced.16,17
Treating bladder cancer takes a team effort, and several healthcare professionals will become involved in your treatment plan. Treatment efforts are based on your unique circumstances and the stage of the cancer.18
For many people, surgery becomes the main treatment option.19 The type of surgery offered usually depends on the location of bladder cancer and can include:
Like any type of surgery, cystectomy comes with risks that depend on the extent of the operation. Some risks may include but aren’t limited to:20
Doctors typically recommend this type of treatment for early-stage bladder cancers isolated in or very close to the bladder lining. In some cases, doctors suggest this therapy after TURBT to help lower the risk of tumors returning later.21
During this procedure, a doctor injects a medication directly into the bladder using a catheter that’s inserted through the urethra. The medication used may be a chemotherapeutic agent, or it may be an immunotherapy medicine.21
During radiation treatment, high-energy radiation particles directly target cancer cells to kill them. People often receive radiation along with chemotherapy (chemoradiation) to help the radiation treatment work better.22
Generally, people living with bladder cancer receive chemotherapy in one of two ways:23
Common chemotherapy drugs include:23
These medicines may be used alone or as a combination of medications to help treat bladder cancer.23
Immunotherapy harnesses the power of the body’s own immune system to help fight cancer. Patients typically receive these medications in one of two ways:24
Targeted therapies directly affect specific parts of cancerous cells to prevent them from growing. They include:26

According to the World Health Organization, bladder cancer is the ninth most common type of cancer affecting people around the world. In 2022, over 600,000 people worldwide received a bladder cancer diagnosis and, of those, more than 220,000 people died from the disease.27
Bladder cancer is unfortunately usually difficult and expensive to diagnose and treat. Cystoscopy is a main diagnostic method, but the procedure is expensive and invasive.27
Fortunately, doctors often diagnose bladder cancer in the initial stages, when it’s more likely to respond well to treatment. Only about 25 percent of bladder cancers are first discovered in later stages of the disease.27
To date, there isn’t much evidence linking the causative relationship between urinary tract infections and bladder cancer. However, at least one study associates recurrent UTIs as a risk factor for genitourinary cancers including genital, kidney, and bladder cancer, especially in people assigned male at birth.28
While urinary infections and other causes of chronic bladder irritation have been associated with bladder cancer, it is not clear whether they cause bladder cancer.8 Unfortunately, bladder cancer symptoms often mimic those of other conditions like UTIs, overactive bladder, or an enlarged prostate.11,12
Some research suggests that people assigned female at birth could have a delayed diagnosis of bladder cancer if they regularly receive treatment for UTIs. This could be because healthcare providers may not investigate for cancer because they assume symptoms are related to another UTI.29
The outcomes of bladder cancer treatment depend on many factors, such as the stage and grade of the cancer, the type of cancer diagnosed, and the patient’s overall health and age. Survival rates for muscle-invasive bladder cancer also depend on the presence or absence of carcinoma in situ.30
Five-year survival rates highlight the percent of people living with the same type and stage of bladder cancer that are alive five years after receiving a diagnosis. Currently, the 5-year survival rates for bladder cancer are:30
The exact causes of bladder cancer are unknown.7 Risk factors that could make a person more likely to develop bladder cancer include smoking and exposure to certain chemicals.3,6
Research suggests people who smoke are at least three times more likely to develop bladder cancer. People working in industries that produce products like rubber, leather, printing materials, textile, and paint, as well as specific occupations such as firefighters and hairdressers, are also at higher risk.8
Symptoms of bladder cancer often resemble those of other medical conditions, like UTIs, bladder or kidney stones, overactive bladder, or an enlarged prostate. In most cases, blood in the urine is the first symptom noticed.11,12
Squamous cells are a type of epithelial cell that can be found in urine. It’s normal for a small number of squamous cells to appear—however, a larger number could indicate a UTI or yeast infection, or a more serious condition like cancer.31
For people of average risk, there is no current standard method to screen for bladder cancer.32 If your doctor suspects cancer, they will perform several tests to arrive at a diagnosis. These tests usually include taking a medical history and performing a physical examination, which may include a digital rectal examination. Other tests, like urine lab tests, biopsy, and imaging tests are also usually recommended.14,15
After making a diagnosis, your doctor will stage the cancer to determine if and how far it’s spread beyond the bladder. Then, your treatment team creates a plan based on various factors, like the extent of the cancer, your overall health, and more.18
Find a Pfizer trial for bladder cancer at PfizerClinicalTrials.com
Explore bladder cancer clinical trials at ClinicalTrials.gov
Area of Focus: Oncology
Bladder Cancer is a focus area for Pfizer Oncology. To learn more about how we’re accelerating breakthroughs to outdo cancer, visit the Oncology page.
Find resources for those living with cancer and their caregivers at This is Living with Cancer.
The information contained on this page is provided for your general information only. It is not intended as a substitute for seeking medical advice from a healthcare provider. Pfizer is not in the business of providing medical advice and does not engage in the practice of medicine. Pfizer under no circumstances recommends particular treatments for specific individuals and in all cases recommends consulting a physician or healthcare center before pursuing any course of treatment.