- Home
- Science
- Diseases & Conditions
- Cardiovascular Disease
What Is Cardiovascular Disease?
The umbrella category of cardiovascular disease includes a spectrum of disorders of the heart and blood vessels, including coronary artery disease (CAD), cerebrovascular disease, and certain congenital issues. Many types of cardiovascular disease carry no symptoms until a heart attack or stroke reveals an underlying condition.1
Prevalence of Cardiovascular Disease
Though largely preventable, cardiovascular disease still ranks as the leading cause of death both in the U.S. and globally.1,2 In the U.S., heart disease killed 696,962 people in 2020. That’s 211.5 deaths per 100,000 people, or approximately 1 in every 3 deaths in the U.S. every year.2,3
However, its impact can be lessened by cardiovascular disease management interventions, including early detection, lifestyle changes (diet and exercise) and medication.1
PfizerForAll

Pfizer is fighting for 8 cancer breakthroughs by 2030
We're driving the breakthroughs of tomorrow while fighting against cancer today. The fight takes all of us. Start by answering a few questions to understand your own cancer risks at PfizerForAll.com.
Get Started DetailsTypes of Cardiovascular Disease
Cardiovascular disease is not one condition. It’s a parent term for all diseases that affect the blood vessels or heart, including heart failure, stroke, and peripheral artery disease.1
Not all cardiovascular diseases are described as heart disease. In most cases, when someone says “heart disease,” they're referring to coronary heart disease.3 Common types of cardiovascular disease include:2,4,5,6,7,8
- CAD, a blood vessel disease
- Heart rhythm problems, known as arrhythmia
- Congenital heart defects (CHDs), which are present at birth
- Heart valve disease
- Disease of the heart muscle, or cardiomyopathy
- Inflammation of the heart caused by infections

Coronary Artery Disease
In the United States, coronary artery disease is the most common form of heart disease.4 Also known as ischemic heart disease or coronary heart disease, CAD may be revealed first in many people by a heart attack.4 Approximately 20.1 million U.S. adults aged 20 and older have CAD.9
- What Causes Coronary Artery Disease?
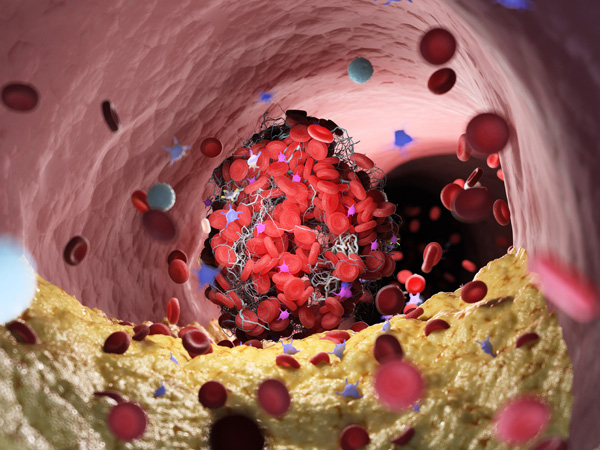
CAD happens when plaque (deposits of substances like cholesterol) builds up in the walls of the arteries that supply the heart and other parts of the body with blood.4 Over time, the buildup causes the arteries to narrow, partially or completely blocking the flow of blood. This development is known as atherosclerosis.4
- Coronary Artery Disease Risk Factors
There are a number of major risk factors for coronary heart disease.
A family history of CAD increases the risk for the condition, especially a history of heart disease under the age of 50.4 Other risk factors include carrying excess body fat, not getting enough physical activity, smoking tobacco, and having unhealthy eating habits.4
High blood pressure is another significant risk factor for heart disease.10 This condition happens when the pressure of the blood is too high in a person's arteries and other blood vessels. If left uncontrolled, the pressure can eventually affect the heart and other major organs, including the brain and kidneys. High blood pressure has gained a reputation as a “silent killer,” because it generally doesn't have symptoms. However, checking your blood pressure can help you monitor your levels.10
Cholesterol is a major culprit in CAD. Cholesterol is a type of fat (also known as “lipid”) found in the bloodstream.11 High levels of cholesterol increase the risk for heart disease (heart attack) or stroke. This is because fatty deposits in the blood vessels can build up and block the blood flow to and from the heart.11 Cholesterol comes through the liver, which produces cholesterol to meet the body’s needs, and diet. The most important culprit in the diet are foods high in saturated fat, such as fatty meats and other sources of animal fat.11,12
There are two general classes of cholesterol.10 Non-high-density lipoprotein (non-HDL) cholesterol, of which low-density lipoprotein (LDL) cholesterol is the most known subtype, is generally called “bad” cholesterol because it can cause plaque buildup in arteries. In contrast, high-density lipoprotein (HDL) cholesterol, the “good” cholesterol, protects against heart disease.10,12
Obesity is another risk factor for CAD. Obesity is linked to higher levels of “bad” cholesterol and triglycerides (the other major type of lipid, or blood fat). Obesity is also linked to lower “good” cholesterol levels.10
Diabetes is also a risk factor for coronary artery disease. People with diabetes have a higher risk of death from heart disease than those without the condition. CAD is the leading cause of death for people with diabetes.13
Tobacco use is another major risk factor for CAD. People are often aware of the link between tobacco use and lung cancer but may not know the link to heart attack.10
Additional risk factors for CAD include genetic profile and ethnicity.10 For American Indians, white and Black Americans, and Alaska Natives, heart disease is the leading cause of death. For Asian Americans, Hispanics, and Pacific Islanders, it’s second only to cancer. Heart disease is the number one killer of both men and women, and risk grows with increasing age. Still, CAD can develop at any age.9,10
- Coronary Artery Disease Symptoms
The most common symptom of CAD is angina, or chest discomfort and pain.4 Experienced by an estimated 9 million Americans each year, angina happens when excessive plaque builds up in the arteries.4,14 But for many, the first indication of narrowing arteries is a heart attack, the symptoms of which include:4
- Nausea, weakness, a cold sweat, or light-headedness
- Shortness of breath
- Pain or discomfort in the arms or shoulders
If CAD persists, it can weaken the heart muscle. This can lead to heart failure as the heart loses the ability to pump blood properly.4 - Coronary Artery Disease Treatment
CAD treatment hinges on the severity of symptoms and the presence of other health conditions. Healthcare providers generally advise CAD patients to maintain a healthy weight, stay physically active, eat a heart-healthy diet (like the DASH), practice stress management, quit tobacco, and get sufficient sleep.15
Doctors may also prescribe certain medications, which may reduce other contributors to CAD. These prescriptions can include:15
- Medicines to control blood pressure. These include beta blockers, ACE inhibitors, and calcium channel blockers.
- Medicines to control cholesterol and other blood fats. These include statins and cholesterol absorption inhibitors.
- Medicines to control blood sugar for those who have diabetes. These include SGLT2 inhibitors and GLP1 receptor agonists
- Coronary Artery Disease Prevention
Living a healthier life with coronary artery disease often involves eating a diet that is low in sodium and saturated fat, maintaining a healthy weight, quitting smoking, and increasing exercise.4 Doctors may also recommend treating risk factors such as high blood pressure, irregular heartbeat, and high cholesterol.4
Arrhythmia
Arrhythmia is a problem with the rhythm or rate of a person's heartbeat.5 The heart either beats too slowly, known as bradycardia, or it beats too quickly, known as tachycardia. In some cases, the heart beats in an irregular pattern. The most common form of arrhythmia is atrial fibrillation, a condition that causes a fast and irregular heartbeat.5
- What Causes Arrhythmia?
Multiple factors may lead to arrhythmias, including congenital heart defects, stress, and heart attack.5 Some medications and substances can cause arrhythmias, as well.5
- Arrhythmia Risk Factors
Although some changes in heart rhythm and heart rate are normal, certain people are at higher risk for arrhythmia.16 At-risk populations include people with some form of heart disease, older people, and people with congenital conditions (like being born with extra electrical pathways). Some chemical agents can also cause arrhythmias, including substances like alcohol, cigarettes, and recreational drugs.16
- Arrhythmia Symptoms
Symptoms of arrhythmias include:5
- Slow or fast heartbeat
- The heart skipping beats
- Chest pain
- Dizziness or light-headedness
- Sweating
- Shortness of breath
Holter monitors, transtelephonic monitors, and treadmill testing are all used to check for arrhythmia.17,18 - Arrhythmia Treatment
A variety of treatments for arrhythmias exist, including medications, therapies, surgery, and other medical procedures.19 Medications can help regulate the heart rate. Therapies include vagal maneuvers—which can help stop some arrhythmias by affecting the vagus nerve—and cardioversion, a procedure that resets the heart’s rhythm. Other procedures and surgeries to correct arrhythmias include catheter ablation and the maze procedure, both of which create small scars on the heart to correct irregular beating.19,20 Implantable cardioverter-defibrillators and pacemakers can correct arrhythmias. A person can also lower their arrhythmia risk by addressing the overall risk for heart disease.19
Congenital Heart Defects
Congenital heart defects are heart problems that a person is born with.21
- What Causes Congenital Heart Defects?
In most cases, the causes of CHDs are unknown. Some may stem from alterations to genes or chromosomes, while some may be the result of genetics and other factors, including medication use during pregnancy, a mother’s health conditions, or environmental elements.21
During pregnancy, several health conditions can increase the odds of CHDs. They include:22
- Diabetes acquired before pregnancy, or within the first three months of pregnancy. Controlling blood glucose levels during pregnancy can lower risks for the unborn child.
- Phenylketonuria, which is an inherited disorder that affects how the body metabolizes protein.
- Coming down with rubella (also known as German measles) during pregnancy.
Other environmental factors encountered during pregnancy can increase the chances of a child having a CHD, such as:22- Smoking or exposure to secondhand smoke
- Certain blood pressure and acne medications
A family history of CHDs, including having a child with the condition, may increase the chances of an unborn child having a CHD.22 - Congenital Heart Defects Risk Factors
Research has identified several other risk factors for CHDs:23
- Age of mother: CHDs tend to be more common when the mother is between 20-30 years old or over age 30, compared with those under age 20.
- Age of father: There’s an increased risk of CHD when the father is over age 25.
- Certain illnesses during the first trimester: Febrile illnesses in the mother were associated with an increase in the number of children born with CHDs.
- Lost pregnancies or still births: Previously losing a pregnancy or having a stillbirth were linked to a greater likelihood of CHD.
- Congenital Heart Defects Symptoms
Congenital heart defects can have few or no signs or symptoms. They frequently go undiagnosed until children are older. Signs include rapid breathing, a bluish tint to the skin, poor circulation, and fatigue.22
- Congenital Heart Defects Treatment
Treatment for CHDs varies. Some children do not need treatment at all.22 However, addressing a CHD may involve medication, catheter procedures, or other types of surgery.
- Congenital Heart Defects Prevention
Congenital heart disease generally can't be prevented. But pregnant people should talk to a doctor before taking any medicine and should discuss the types of chemicals or substances that could harm a baby's development. It’s helpful to control blood sugar levels. And it’s also helpful to take a blood test early in the pregnancy to check for rubella and determine vaccination needs.24
Heart Valve Problems
Heart valve problems can be overwhelming. Thankfully, they are often treatable.6 They are frequently first identified by hearing a heart murmur. Murmurs often sound like “whooshing” noises as blood moves between chambers of the heart. They can also sound like an extra click as a valve allows blood to flow backward.6 While some murmurs are harmless, others can point to problems with the valve. These problems include:6
- Stenosis. Narrowing or stiffening of the valve.
- Prolapse. A valve with leaflets that don't close properly.
- Atresia. A valve that has not formed properly or is missing.
- Regurgitation. When a valve or valves allow blood flow back into the previous chamber.
- What Causes Heart Valve Problems?
Valve problems often stem from congenital defects, such as aortic valve stenosis, pulmonary valve stenosis, and bicuspid aortic valve.6 They can also be caused by age-related factors, including degenerative valve disease and calcification.6
Valve issues also may be associated with conditions and illnesses, such as infective endocarditis, rheumatic fever, and blunt-force injuries from car accidents.6,25
- Risk Factors for Heart Valve Problems
People who received radiation to the chest (mediastinal radiation therapy) have an increased risk for valve disease in older age.6 For example, studies have shown that childhood cancer survivors who had radiation therapy are in this group.6
- Symptoms of Heart Valve Problems
Heart valve disease often presents no distinct symptoms, making checking for symptoms even more important. Chest pain, light-headedness, shortness of breath, and fatigue can be signs of several conditions and may point to heart valve disease.26
- Heart Valve Problems Treatment
With proper treatment, there is a promising chance of recovering from heart valve problems.27 Some people with mild problems never need surgery and live long and full lives. That said, once a valve begins to affect the heart's ability to pump, it will likely need repair or replacement. Doctors may call for open-heart surgery or a minimally invasive procedure, such as a transcatheter aortic valve replacement or transcatheter aortic valve implantation.27
- Prevention of Heart Valve Problems
Researchers are currently examining whether cholesterol-lowering medication can help prevent aortic stenosis, the stiffening and thickening of the aortic valve.28
If signs of a strep infection appear, see a doctor and check for valve disease caused by rheumatic fever. Treating these infections helps prevent rheumatic fever, which can damage the heart's valves.29
Cardiomyopathy
Cardiomyopathy describes any disorder that affects the heart muscle, causing it to lose its ability to properly pump blood.7 In some cases, cardiomyopathy can also lead to arrhythmias. Three types of cardiomyopathy typically affect adults: hypertrophic, dilated, and restrictive.7
Cardiomyopathy is distinct from other heart disorders in a few ways:
- It can occur in young people.7
- It tends to be progressive.7
- It can be associated with diseases involving other organs.7
- It's frequently the result of gradual changes of the heart structure over extended periods of time.7
- It's a leading cause of heart transplants.30
- What Causes Cardiomyopathy?
There are multiple causes of cardiomyopathy, including:7
- Diseases that affect the connective tissues as well as autoimmune disease
- Heart attack or coronary heart disease
- Heart-damaging diseases, such as amyloidosis, sarcoidosis, or hemochromatosis
- Diseases of the endocrine system, such as diabetes and thyroid conditions
- Heart-muscle infections
- Alcohol or cocaine abuse
- Diseases that affect the muscles, such as muscular dystrophy
- Pregnancy
- Cardiomyopathy Risk Factors
Certain infections, such as viral hepatitis and HIV, are risk factors for cardiomyopathy. Very stressful situations can also lead to a specific form of the condition called takotsubo cardiomyopathy, which is also known as broken-heart syndrome.31 A family history of sudden cardiac arrest, heart failure, or cardiomyopathy represents another risk factor.7
- Cardiomyopathy Symptoms
Symptoms of cardiomyopathy vary depending on type. They include:32
- Fatigue
- Trouble breathing during exertion
- Heart palpitations
- Fainting after physical activity
- Dizziness
- Chest pains
- Cardiomyopathy Treatment
Many people with cardiomyopathy have no signs or symptoms and ultimately might not need treatment.32 For example, dilated cardiomyopathy that appears suddenly may go away on its own. For those who do need treatment, following a treatment plan can help control symptoms, manage medical conditions, and reduce complications, such as the risk for sudden cardiac arrest. Treatments may include:33
- Lifestyle changes
- Nonsurgical procedures
- Medication to balance electrolytes, lower blood pressure, and reduce inflammation
- Surgery, such as septal myectomy, and implanted devices, like a cardiac resynchronization therapy device
- Cardiomyopathy Prevention
Inherited types of cardiomyopathy can't be prevented.7 However, people can lower the risk for the diseases and conditions that lead to cardiomyopathy, such as high blood pressure and heart attack.7,34 Avoiding alcohol, cocaine, and amphetamines; forming better eating habits; managing stress; and quitting smoking can all benefit the heart.31
Endocarditis
Endocarditis—an inflammation of the lining of the heart valves and heart chambers (endocardium)—is caused by an infection of the heart.8
- What Causes Endocarditis?
Endocarditis happens when germs travel to the heart after entering the bloodstream.8 Although a bacterial infection is the most common culprit, fungi such as Candida can also cause the condition. However, sometimes, no cause is found.8
Germs are most likely to enter the bloodstream through central venous access lines, dental surgery, or injection drug use.8 Germs can also enter the bloodstream through surgeries or procedures to the urinary or breathing tracts, or through infected bones, skin, and muscles.8
- Endocarditis Risk Factors
People who develop endocarditis sometimes have birth defects, damaged heart valves, long-term intravenous (IV) lines, new heart valves after surgery, or a history of endocarditis.8
- Endocarditis Symptoms
The symptoms of endocarditis can come on suddenly or develop slowly. They often include chills, fever, and sweating, which can begin days before other symptoms appear.8 They can come and go. And they are often more noticeable at night.8
People with endocarditis may also feel weakness, fatigue, and aches and pains in joints or muscles.8 Other signs include painless red spots on the palms and soles known as Janeway lesions, small areas of bleeding under the nails called splinter hemorrhages, painful red nodes on finger and toe pads known as Osler nodes, and swelling in the legs, feet, and abdomen.8
- Endocarditis Treatment
Treatment for endocarditis may involve going to a hospital for IV antibiotics. Patients sometimes need long-term antibiotic therapy—typically for four to six weeks—to eliminate all bacteria from the heart’s valves and chambers. Antibiotic treatments that start in the hospital continue once a patient is home. In many cases, a valve will need to be replaced if the infection is breaking apart (causing strokes), if the patient develops heart failure, or if there's evidence of more severe organ damage. Getting treatment for endocarditis immediately will improve the chances of a positive outcome.8
- Endocarditis Prevention
The American Heart Association recommends preemptive antibiotics for people at high risk for endocarditis.8 This includes people with certain birth defects, heart transplant and valve problems, a history of endocarditis, and prosthetic heart valves.8
Cardiovascular Disease Diagnosis
Diagnosing all types of heart disease involves a range of tests, both invasive and noninvasive. Doctors frequently begin by exploring personal and family medical histories, discussing symptoms, ordering blood tests and an electrocardiogram (EKG/ECG), which is a recording of the heart’s electrical activity. Depending on the results, doctors may order additional testing or refer the patient to a cardiologist.35,36
- Laboratory Tests for Cardiovascular Disease
Lab tests have been widely used in medicine for decades to identify the presence or elevated levels of certain substances that are indicative of specific health conditions. Lab tests can also determine whether a person is at risk of developing certain health conditions in the future. Specific blood tests can check for the presence of cardiovascular disease and cardiovascular disease risk.36
- Lipid profile for total cholesterol, LDL, HDL, and triglycerides.36
- Lipoprotein (a), or Lp (a), can help determine future or current risk of atherosclerosis.36
- C-reactive protein, if elevated, can be indicative of an increased risk of cardiac health issues.36
- Homocysteine, which the body uses to make protein. If too much is present, you may have an increased risk for heart disease and stroke. This test is usually ordered for people who have a high risk for heart disease, who have a known history of heart disease, or who have conditions such as high blood pressure, high cholesterol, or diabetes.37
- Blood Tests for Other Bodily Systems
Although the following blood tests are not directly related to the heart, they provide information about other bodily systems that may have an impact on cardiovascular health. These include:
- Complete blood count, which measures red and white blood cells and platelets.38
- Checking sodium and potassium levels, which can reveal problems with electrolytes in bodily fluids.39
- Checking blood urea nitrogen and creatinine, which helps evaluate kidney function.40
- A fasting glucose test, which can help diagnose diabetes.41
- Alanine transaminase42 and aspartate aminotransferase tests,43 which can indicate damage to or inflammation of the liver.
- Thyroid-stimulating hormone tests, which check thyroid function.44
- Noninvasive Tests for Cardiovascular Disease
Fortunately, several noninvasive tests can assess whether a person has cardiovascular disease. These include:
- EKG or ECG. This test measures the electrical activity of the heart. An EKG or ECG will also show heart rate and whether the heart is beating steadily or irregularly.45
- Echocardiogram. In this test, sound waves show the heart in motion, which can shed light on the function of the heart’s valves and chambers.45
- Stress tests. These tests evaluate how a person's heart performs under physical stress, which is usually created by exercising on a treadmill or bicycle. If a person cannot use either of these, medication can help simulate the ways a heart reacts to exercise.45
- Holter monitor. Patients wear this portable machine for 24 to 48 hours. It continuously records patients’ EKGs as they go about their daily lives. During the test, a patient is asked to keep a log of symptoms and activities. The test can also catch arrhythmias that might not be recorded by a resting EKG.17,46
- Invasive Tests for Cardiovascular Disease
In some cases, it is necessary for doctors to take a closer look at the heart to treat cardiovascular disease. The good news is that invasive tests are sometimes accompanied by some type of corrective action aimed at restoring normal function to the heart. These invasive tests include45,47:
- Cardiac catheterization. This helps diagnose—and in some cases even treat—heart disease by opening blocked arteries through balloon angioplasty and stent placement. For this test, a cardiologist inserts a long, flexible catheter into a blood vessel through the wrist or groin, guiding it toward the heart with the help of an X-ray. Once in place, doctors perform other tests to evaluate blockages and heart function.45,48,49
- Electrophysiology study. This recording of the heart's electrical activity helps doctors identify the cause of arrhythmias and determine the best treatments. Doctors can also use this test to reproduce an arrhythmia and determine which medications will control it best.47
Global Impact of Cardiovascular Diseases

The World Health Organization reported that nearly 18 million people worldwide died from cardiovascular disease in 2019, accounting for 32% of all deaths.1 Of those deaths, 85% resulted from heart attack and stroke. However, these deaths are not evenly distributed around the world. Over three-quarters of them occur in low-and middle-income countries.1
On the global front, cardiovascular disease caused 38% of deaths due to noncommunicable diseases of people under the age of 70 in 2019.1 Most cardiovascular diseases can be prevented by tackling behavioral risk factors, including unhealthy diets, physical inactivity, harmful use of alcohol, and tobacco use. Early detection is also incredibly important for effectively managing the conditions with medicine and counseling.1
It is possible to reduce the disease burden of cardiovascular conditions. Evidence from 18 countries demonstrated that efficient hypertension programs at the primary care level can help reduce stroke and coronary heart disease.1
Frequently Asked Questions About Cardiovascular Disease
- Is hypertension a cardiovascular disease?
Hypertension is a type of cardiovascular disease and can contribute to reduced blood flow to the heart and stroke. That’s why doctors advise identifying and treating hypertension early.50
- Is stroke a cardiovascular disease?
Yes. Stroke is a type of cardiovascular disease.51
- How does aerobic exercise prevent cardiovascular disease?
In general, physical activity improves heart health and therefore lowers cardiovascular disease risk. Evidence suggests that frequent exercise decreases the risk of developing or dying from death cardiovascular disease. Regular exercise leads to healthier cholesterol levels, decreases the likelihood of diabetes, and lowers blood pressure. While exercise increases heart rate and blood pressure in the moment, people who exercise regularly adapt and have overall lower resting heart rates.52
- How many people die from cardiovascular disease?
In the United States, one person dies every 34 seconds from cardiovascular disease.9 In 2017-2018, the toll of cardiovascular disease cost the country about $229 billion every year in medicine, healthcare services, and lost productivity. Heart disease causes 211.5 deaths for every 100,000 people. That’s about 1 in 3 deaths annually in the U.S.9
- When my heart skips a beat, is that dangerous?
Heart palpitations can feel like the heart is racing, pounding, or skipping or missing beats. These sensations may occur in the neck, throat, or chest. People with a known heart disease, risk factors for heart disease, an abnormal heart valve, or an electrolyte imbalance, such as a low level of potassium, may experience heart palpitations.53 Medications, caffeine, and anemia are among the many potential causes of heart palpitations.54 A heartbeat that is too fast, too slow, or inconsistent may also be indicative of arrythmia. In addition to the feeling of skipped beats, people experiencing arrythmia may feel lightheaded or dizzy, experience chest pain, have shortness of breath, or sweat.5
Learn More About Cardiovascular Disease
Find a Pfizer cardiovascular disease clinical trial at PfizerClinicalTrials.com.
Explore cardiovascular disease clinical trials at ClinicalTrials.gov.
Area of Focus: Internal Medicine
Cardiovascular Disease is a focus of Pfizer’s Internal Medicine Therapeutic Area. Visit the Internal Medicine Page.
- References
- Cardiovascular diseases. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Published June 11, 2021. Accessed February 17, 2022.
- Heart disease. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/fastats/heart-disease.htm. Published February 1, 2022. Accessed February 17, 2022.
- Know the difference: cardiovascular disease, heart disease, coronary heart disease. National Institutes of Health. https://www.nhlbi.nih.gov/sites/default/files/publications/FactSheetKnowDiffDesign2020V4a.pdf. Accessed February 17, 2022.
- Coronary artery disease. Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/coronary_ad.htm. Published July 19, 2021. Accessed February 17, 2022.
- Arrhythmia | irregular heartbeat. MedlinePlus. https://medlineplus.gov/arrhythmia.html. Published July 9, 2021. Accessed February 17, 2022.
- Heart valve problems and causes. https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-problems-and-causes. Published May 8, 2020. Accessed February 17, 2022.
- Cardiomyopathy. https://www.cdc.gov/heartdisease/cardiomyopathy.htm. Centers for Disease Control and Prevention. Updated December 9, 2019. Accessed October 13, 2022.
- Endocarditis. MedlinePlus. https://medlineplus.gov/ency/article/001098.htm. Published February 4, 2022. Accessed February 17, 2022.
- Tsao CW, Aday AW, Almarzooq ZI, Beaton AZ, Bittencourt MS, Boehme AK, et al. Heart Disease and Stroke Statistics—2022 Update: A Report From the American Heart Association. Circulation. 2022;145(8):e153–e639.
- Know your risk for heart disease. Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/risk_factors.htm. Published July 19, 2019. Accessed February 17, 2022.
- About cholesterol. Centers for Disease Control and Prevention. https://www.cdc.gov/cholesterol/about.htm. Updated June 24, 2021. Accessed October 13, 2022.
- What is cholesterol? American Heart Association. https://www.heart.org/en/health-topics/cholesterol/about-cholesterol. Updated November 6, 2020. Accessed October 13, 2022.
- Aronson D, Edelman ER. Coronary artery disease and diabetes mellitus. Cardiology Clinics. 2014;32(3):439-455.
- Angina. StatPearls. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK557672/. Updated December 21, 2021. Accessed October 13, 2022.
- Coronary heart disease treatment. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/coronary-heart-disease/treatment. Updated March 24, 2022. Accessed October 13, 2022.
- Understand your risk for arrhythmia. www.heart.org. https://www.heart.org/en/health-topics/arrhythmia/understand-your-risk-for-arrhythmia. Published September 30, 2016. Accessed February 17, 2022.
- Common tests for arrhythmia. heart.org. https://www.heart.org/en/health-topics/arrhythmia/symptoms-diagnosis--monitoring-of-arrhythmia/common-tests-for-arrhythmia. Published September 6, 2016. Accessed February 17, 2022.
- Special heart rhythm testing. American Heart Association. http://m.heart.org/idc/groups/heart-public/@wcm/@hcm/documents/downloadable/ucm_317648.pdf. Accessed December 1, 2022.
- Arrhythmias. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/arrhythmias/treatment. Update March 24, 2022. Accessed October 14, 2022.
- Weimar T, Schena S, Bailey MS, et al. The cox-maze procedure for lone atrial fibrillation: a single-center experience over 2 decades. Circ: Arrhythmia and Electrophysiology. 2012;5(1):8-14.
- What are congenital heart defects? Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/heartdefects/facts.html. Updated January 24, 2022. Accessed October 14, 2022.
- Congenital heart defects. MedlinePlus. https://medlineplus.gov/congenitalheartdefects.html. Published November 29, 2021. Accessed February 17, 2022.
- Abqari S, Gupta A, Shahab T, Rabbani M, Ali Sm, Firdaus U. Profile and risk factors for congenital heart defects: A study in a tertiary care hospital. Ann Pediatr Card. 2016;9(3):216.
- Congenital heart disease. familydoctor.org. https://familydoctor.org/condition/congenital-heart-disease/. Accessed February 17, 2022.
- Esmaeilzadeh M, Alimi H, Maleki M, Hosseini S. Aortic valve injury following blunt chest trauma. Res Cardiovasc Med. 2014;3(3):2.
- Heart valve disease risks, signs and symptoms. www.heart.org. https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-disease-risks-signs-and-symptoms. Published May 11, 2020. Accessed February 17, 2022.
- Understanding your heart valve treatment options. www.heart.org. https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/understanding-your-heart-valve-treatment-options. Published May 11, 2020. Accessed February 17, 2022.
- Nsaibia MJ, Devendran A, Goubaa E, Bouitbir J, Capoulade R, Bouchareb R. Implication of lipids in calcified aortic valve pathogenesis: Why did statins fail? JCM. 2022;11(12):3331.
- Rheumatic fever: all you need to know. Centers for Disease Control and Prevention. https://www.cdc.gov/groupastrep/diseases-public/rheumatic-fever.html. Last reviewed November 1, 2018. Accessed June 2, 2022.
- Everly MJ. Cardiac transplantation in the United States: An analysis of the UNOS registry. Clin Transpl. 2008:35-43. PMID: 19708444.
- Cardiomyopathy causes and risk factors. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/cardiomyopathy/causes. Updated March 24, 2022. Accessed 14, 2022.
- Cardiomyopathy. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/cardiomyopathy. Accessed February 17, 2022.
- Prevention and treatment of cardiomyopathy. American Heart Association. https://www.heart.org/en/health-topics/cardiomyopathy/prevention-and-treatment-of-cardiomyopathy. Last reviewed May 5, 2022. Accessed June 2, 2022.
- Cardiomyopathy. MedlinePlus. National Library of Medicine. https://medlineplus.gov/cardiomyopathy.html#cat_42. Accessed October 17, 2022.
- Heart disease. Medline Plus. National Library of Medicine. https://medlineplus.gov/heartdiseases.html. Last reviewed September 2, 2022. Accessed October 17, 2022.
- Adams J, Apple F. New blood tests for detecting heart disease. Circulation. 2004;109(3).
- Homocysteine test. Medline Plus. National Library of Medicine. https://medlineplus.gov/lab-tests/homocysteine-test/. Updated September 28, 2022. Accessed October 17, 2022.
- Madjid M, Fatemi O. Components of the complete blood count as risk predictors for coronary heart disease: in-depth review and update. Tex Heart Inst J. 2013;40(1):17-29.
- Sodium, potassium and health. Centers for Disease Control and Prevention. https://www.cdc.gov/salt/potassium.htm. Updated August 23, 2022. Accessed October 17, 2022.
- Brisco MA, Coca SG, Chen J, et al. Blood urea nitrogen/creatinine ratio identifies a high-risk but potentially reversible form of renal dysfunction in patients with decompensated heart failure. Circ: Heart Failure. 2013;6(2):233-239.
- Park C, Guallar E, Linton JA, et al. Fasting glucose level and the risk of incident atherosclerotic cardiovascular diseases. Diabetes Care. 2013;36(7):1988-1993.
- Ndrepepa G, Kastrati A. Alanine aminotransferase—a marker of cardiovascular risk at high and low activity levels. J Lab Precis Med. 2019;4:29-29.
- Ndrepepa G. Aspartate aminotransferase and cardiovascular disease—a narrative review. J Lab Precis Med. 2021;6:6-6.
- Kannan L, Shaw PA, Morley MP, et al. Thyroid dysfunction in heart failure and cardiovascular outcomes. Circ: Heart Failure. 2018;11(12):e005266.
- Heart health tests. Medline Plus. National Library of Medicine. https://medlineplus.gov/hearthealthtests.html. Updated February 28, 2017. Accessed October 17, 2022.
- Holter monitor. American Heart Association. https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/holter-monitor. Updated July 31, 2015. Accessed October 17, 2022.
- Majeed H, Sattar Y. Electrophysiologic study indications and evaluation. StatPearls. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK567719/. Updated January 14, 2022. Accessed October 17, 2022.
- Cardiac catheterization. American Heart Association. https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/cardiac-catheterization. Updated July 31, 2015. Accessed December 1, 2022.
- Heart procedures and surgeries. American Heart Association. https://www.heart.org/en/health-topics/heart-attack/treatment-of-a-heart-attack/cardiac-procedures-and-surgeries. Updated October 5, 2020. Accessed December 1, 2022.
- Tackling G, Borhade M. Hypertensive heart disease. StatPearls. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK539800/. Updated June 27, 2022. Accessed October 17, 2022.
- What is cardiovascular disease? American Heart Association. https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease. Accessed October 17, 2022.
- Nystoriak MA, Bhatnagar A. Cardiovascular effects and benefits of exercise. Front Cardiovasc Med. 2018;5:135.
- Heart palpitations. MedlinePlus. National Library of Medicine. https://medlineplus.gov/ency/article/003081.htm. Accessed October 18, 2022.
- Palpitation. StatPearls. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK436016/. Updated June 17, 2022. Accessed October 18, 2022.
The information contained on this page is provided for your general information only. It is not intended as a substitute for seeking medical advice from a healthcare provider. Pfizer is not in the business of providing medical advice and does not engage in the practice of medicine. Pfizer under no circumstances recommends particular treatments for specific individuals and in all cases recommends consulting a physician or healthcare center before pursuing any course of treatment.