Maternal Immunization
What is Maternal Immunization?
Maternal immunization is a tool to help pregnant women pass on disease-specific antibodies to the fetus during the second and early third trimesters, helping to protect the infant during the most vulnerable time of life—the first six months.1

Enhancing the Power of Maternally Derived Immunity
The immune systems of infants are often not strong enough to protect against infections. Direct active immunization (vaccination provided to the child) is not an option for some life-threatening infectious diseases because infant immune systems are not fully developed and when available, multiple doses are typically required.2 Maternal immunity is a natural phenomenon by which pregnant women provide protection to their vulnerable and growing babies by transferring antibodies through the placenta.1
In order to provide protection, however, enough antibodies need to be passed to the baby. This means that higher antibody levels in the pregnant woman are more likely to lead to increased levels of antibodies in the developing fetus, which can help protect the infant after birth.3 Pregnant women can acquire high levels of antibodies through vaccination.3
Maternal vaccination can help enhance existing maternal immunity by ensuring that pregnant women have enough antibodies to transfer to their babies.3 Additionally, vaccinated pregnant women produce vaccine-specific antibodies that can help better protect infants against specific infections.3 Vaccines against tetanus, influenza, and pertussis have been used during pregnancy for many years to enhance maternal immunity and help protect infants.3

Pfizer’s Innovation in Maternal Vaccines: Furthering a Legacy of Scientific Excellence
Building on decades of expertise and knowledge in pioneering vaccines, Pfizer has developed a maternal immunization for respiratory syncytial virus (RSV) and is currently developing a potential vaccine for Group B streptococcus (GBS).
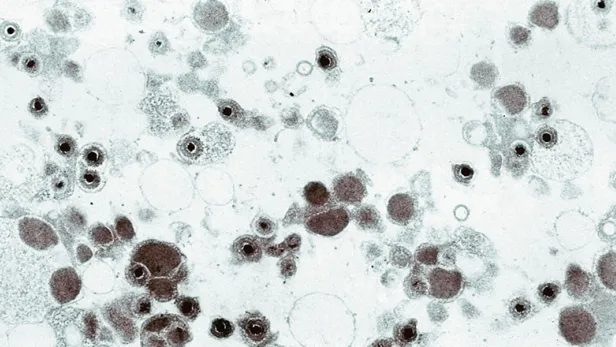
GBS, a common bacterium (an organism that can cause disease), can cause potentially devastating diseases in infants when gestational individuals who carry the GBS bacteria pass them on to their newborns during labor and birth.4 Prevention of invasive infant GBS disease relies upon screening and administration of antibiotics during delivery (known as intrapartum antibiotics or IAP), though many countries do not have the resources to implement IAP and IAP policies are not 100% effective at preventing invasive GBS disease even when correctly implemented.5,6
Strategic Partnerships to Deliver Life Changing Vaccines
Pfizer’s maternal immunization efforts align with our broader commitment to partner with the global health community, including public-private partnerships that may help accelerate global access to our vaccines in the world's poorest countries.
Our longstanding partnership with the Bill and Melinda Gates Foundation, with respect to our maternal immunization program, includes grants to support the continued development of certain aspects of our GBS vaccine candidate, and accessibility of this vaccine candidate, if approved, for those who are pregnant and living in lower-income countries where prevalence of these potentially devastating infections is higher.
What You Need to Know About Maternal Immunization
- Are babies more vulnerable to disease in the first few weeks of life?
The immune systems of infants often are not yet strong enough to defend against all infections. Direct active immunization (vaccination provided to the child) is not an option for some life-threatening infectious diseases because infant immune systems are not yet fully developed.2 Consequently, although an infant’s immune system can fight off most infections, some can be serious or fatal.
- How does maternal immunization work?
To compensate for infants’ still-developing immune systems, nature devised a temporary defense mechanism to help infants fight off infections. Starting in the second trimester, and peaking during the third trimester of pregnancy, antibodies pass from the gestational parent to the growing fetus through the placenta.1 These maternal antibodies are highest in the baby at the time of birth and then gradually decline over the next 6 to 12 months as the baby’s own immune system matures.1 In addition, after birth, antibodies can also be passed to the child through breastfeeding.1 Maternal antibodies can help infants to fight off infections during their most vulnerable time of life—the first six months.1
To provide protection, however, enough antibodies need to be passed to the fetus. This means that higher antibody levels in the gestational parent are more likely to lead to increased levels of antibodies in the developing fetus.3 Those who are pregnant can acquire high levels of antibodies either through a recent exposure to infectious disease or through vaccination. Maternal vaccination may help ensure that those who are pregnant have enough antibodies available to transfer to their babies in hopes of decreasing the infant’s risk of disease and death.3
- How long does maternally derived immunity last?
Antibodies passed to infants during pregnancy are believed to provide immunity until around six months of age, when they’re most vulnerable to infections. Breast feeding can extend a baby’s ability to fight infection by strengthening immunity.1
- What maternal immunization programs are in Pfizer’s development pipeline?
To help reduce the global disease burden in young infants, WHO, the U.S. Food and Drug Administration (FDA), and other regulatory agencies, along with The Bill and Melinda Gates Foundation (BMGF), have recognized the importance of developing vaccines specifically for those who are pregnant.
Pfizer is currently developing a vaccine for Group B streptococcus (GBS), a bacterial illness that can strike within just a few hours or days after birth and has the potential to cause devastating disease.4
Pfizer’s Vaccine Research and Development (R&D) team is actively and passionately working to develop a maternal immunization that has the potential to help prevent GBS disease.
- References
- Faucette A, et al. Immunization of pregnant women: Future of early infant protection. Hum Vaccin Immunother. 2015;11(11):2549-2555. doi:10.1080/21645515.2015.1070984.
- Bergin N, et al. Maternal Vaccination as an Essential Component of Life-Course Immunization and Its Contribution to Preventive Neonatology. Int J Environ Res Public Health. 2018;15(5):847. doi:10.3390/ijerph15050847.
- Vojtek I, et al. Maternal immunization: where are we now and how to move forward?, Ann Med. 2018;50(3):193-208. doi:10.1080/07853890.2017.1421320.
- Goncalves, et al. “Group B streptococcus infection during pregnancy and infancy: estimates of regional and global burden.” Lancet Glob Health 2022. 10: e807–19. https://doi.org/10.1016/S2214-109X(22)00093-6.
- Le Doare K, O'Driscoll M, Turner K, et al. Intrapartum Antibiotic Chemoprophylaxis Policies for the Prevention of Group B Streptococcal Disease Worldwide: Systematic Review. Clin Infect Dis. 2017;65(2):S143-S151. doi:10.1093/cid/cix654.
- Patras KA, Nizet V. Group B Streptococcal Maternal Colonization and Neonatal Disease: Molecular Mechanisms and Preventative Approaches. Front Pediatr. 2018;6:27. doi:10.3389/fped.2018.00027.