How can melanoma be prevented?
Find the answer to this question and ask more at Health Answers by Pfizer.
![]()
Melanoma is a cancer of the skin that forms in skin cells known as melanocytes. These cells give the skin its pigmentation or color. In melanoma, melanocytes enter an uncontrolled growth cycle leading to cancer.1 Types of melanoma skin cancer include cutaneous melanoma, mucosal melanoma, and ocular (uveal) melanoma. Cutaneous melanoma may also be called malignant melanoma, though all melanomas are cancerous even if this word isn’t used.2
Melanoma may begin as a mole or appear on skin that does not have moles.3 When melanoma occurs, it is more likely to spread throughout the body than other types of skin cancer, such as squamous cell carcinoma or basal cell carcinoma.1
People living in parts of the world that receive intense sunlight, like those closer to the equator, tend to experience higher rates of melanoma. Worldwide, incidence rates of melanoma have increased over the past several decades, predominately in fair-skinned people living in North America, Northern Europe, Australia, and New Zealand. Melanoma is comparatively less common in Pacific Island nations, South America, Africa, and Asia.4
The American Cancer Society estimates there will be 104,960 new cases of melanoma in the US in 2025, with 60,550 cases in people assigned male at birth and 44,410 in people assigned female at birth. About 8,430 people are expected to die of melanoma in 2025, including an estimated 5,470 people assigned male at birth and 2,960 people assigned female at birth.5
The prevalence of melanoma differs among age groups in the US. Since the early 2000s, melanoma rates among people assigned female at birth ages 50 and over have increased by 3% each year. Among people assigned male at birth in the same age group, rates stabilized during the same timeframe. In those under 50, rates have been stable for people assigned female at birth, while declining by 1% each year for people assigned male at birth.5
Melanoma mortality rates declined among adults in the US from 2013 to 2022, in large part due to better treatment options.5
Ultraviolet (UV) light is one known cause of melanoma. UV light can come from the sun or from indoor tanning beds and lamps.6
UV light is a carcinogen, meaning it is known to cause cancer. UV light exposure damages DNA inside of skin cells. The body has processes to repair the cells, but mutations may arise once the damage accumulates past a certain point. These mutations can lead to cancer. When mutations accumulate in melanocytes, the resulting cancer is melanoma.6
While UV light is a primary driver of melanoma, there are other causes. Notably, in rare cases, melanoma can be passed down in families.6
Like many diseases, melanoma may affect some people more than others. While anyone can develop melanoma regardless of risk factors, certain risk factors make a person more susceptible to melanoma. These include:6,7
Tanning-bed UV light can be even stronger than the sun.
Hats, pants, and long sleeves can protect skin from the sun, as can applying water-resistant, broad-spectrum sunscreen of sun protection factor (SPF) 30 or higher.8
Melanoma risk increases with age, but younger people can also develop it.
People with these traits tend to have skin that is more sensitive to UV radiation.
Blistering indicates serious damage to skin cells.
Melanoma risk increases when the immune system is weak, which can be caused by certain medical treatments or conditions such as HIV.
While most moles are harmless, certain features of moles carry a higher melanoma risk.
In certain rare instances, melanoma runs in families.
Previous melanoma or other skin cancer indicates that skin was damaged at some point.
These cancers also increase the risk of melanoma.
It’s important to note that having one or multiple risk factors does not guarantee that a person will develop melanoma. Melanoma prevention is important regardless of risk factors.9
People can prevent melanoma by taking precautions to avoid ultraviolet (UV) light exposure. The American Academy of Dermatology advises the following practices to protect the skin and prevent skin cancer:10
UV radiation from the sun is at peak strength from 10 a.m. to 2 p.m. Seek shade when outdoors during these hours.
If you plan to be out in the sun, wear appropriate clothing, including long-sleeved shirts, hats with wide brims, pants, and sunglasses with adequate UV shielding. Clothing with ultraviolet protection factor (UPF) labels offer more effective protection.
Apply sunscreen if you’re venturing outdoors, even when the sky is cloudy. Sunscreen should cover any area that isn’t shielded by clothing. The average adult needs a minimum of one ounce of sunscreen to protect their entire body. Don’t neglect places such as the crown of your head, tops of your ears and feet, and your neck. When choosing a sunscreen, select an option with broad-spectrum protection from UVA and UVB rays. Reapply sunscreen at least every two hours when outdoors or after sweating or swimming.
Tanning bed use can lead to skin cancer. Self-tanning products are a safer alternative. Sunscreen should still be used together with self-tanning products.
All these surfaces can reflect sunlight and lead to sunburn.
When detected early, melanoma is more likely to be treatable. Monitor your skin and see a dermatologist if you notice any new or suspicious spots on the skin, or any spots that itch, bleed, or are changing.11
Melanoma and nonmelanoma are the two main types of skin cancer. Melanoma is rare, while nonmelanoma skin cancer types, such as basal cell carcinoma and squamous cell carcinoma, are more common.12
There are several types of melanoma, including cutaneous melanoma, mucosal melanoma, and ocular melanoma.2 Cutaneous melanoma starts in the skin, while mucosal melanoma occurs in mucous membranes.12 Ocular (also called intraocular or uveal) melanoma forms in eye tissue and is rare.12
There are several subtypes of cutaneous melanoma, including superficial spreading melanoma, nodular melanoma, acral melanoma, and amelanotic melanoma.2 Acral melanoma develops in areas of the body typically not exposed to sunlight, including the palms of the hands, soles of the feet, and underneath the nails.12,13 Amelanotic melanoma is melanoma that does not have the appearance of typical melanomas and can be more difficult to identify.2,14

Generally, melanoma does not resemble skin in the surrounding area. It can take the form of a mole that’s changing or a new age spot or freckle that looks different from nearby areas. Sometimes melanoma has a jagged border.15
Melanoma symptoms typically involve the following:15
Melanoma may be more treatable when detected early. While some people face a greater risk of melanoma, anyone can develop this type of cancer. Self-exams of the skin are a critical step in melanoma detection.10,11
Dermatologists developed the ABCDEs of melanoma to help people identify possible melanoma on the skin:15,16
If the area in question does not divide into two matching halves, take note.
Be alert if the spot's edges are poorly defined, uneven, or notched.
A variety of colors within the spot—such as brown, blue, white, red, or black—can be a warning sign.
While melanomas often exceed 6 millimeters in diameter (roughly pencil eraser size), they may be smaller.
Keep an eye on any alterations in the spot, whether it be in size, shape, or color.
Melanoma and the treatment process may lead to complications, such as:17

Early detection may improve the odds of successfully treating melanoma.10 People who notice changes related to the ABCDEs of melanoma may consider an appointment with a dermatologist. During the appointment, a physician or other healthcare provider may conduct a skin exam, ask about family history of melanoma, and collect general health and symptom information.20
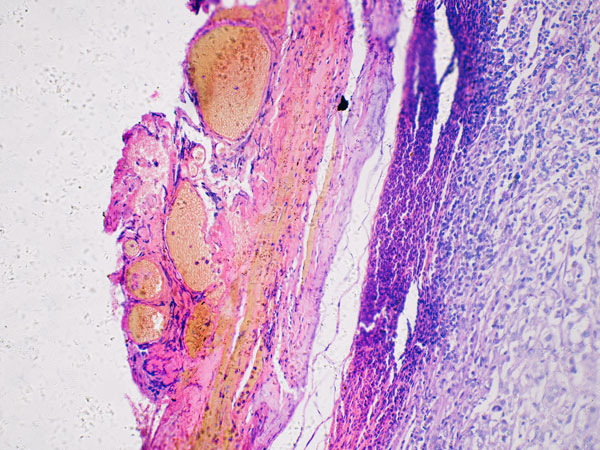
If the dermatologist suspects that the area in question may be cancerous, they may remove part or all of the area and send it to a laboratory for evaluation. This is called a biopsy. A skin biopsy is the only way to know whether the area in question is cancer.20
The dermatopathologist generally shares their findings in a pathology report. If the dermatopathologist finds melanoma, the pathology report will include additional details, such as:20
As with other types of cancer, healthcare professionals stage melanoma to better describe and treat the disease. Cancer staging is a way of communicating information about the cancer, such as whether it has spread to other tissues or the size of the tumor. There are different types of staging systems for cancer.21,22
When staging melanoma, healthcare professionals may use a staging system called the TNM system. TNM is an acronym that classifies melanoma according to three criteria:22
Healthcare professionals examine the tumor to determine how thick it is. If the tumor is less than 1 millimeter thick, the chances of it spreading are lower. Risk of the tumor spreading increases with thickness. Healthcare professionals may also look for ulceration of the tumor. Ulcerated tumors have broken skin on the surface of the melanoma and tend to be more serious.
Clinicians check whether the tumor has reached nearby lymph nodes.
Healthcare professionals investigate whether the tumor has spread beyond the primary tumor into other organs. While melanoma can spread to any part of the body, it tends to affect lymph nodes, the lungs, other parts of the skin, the liver, bones, and the brain.
Doctors may use a simplified staging system to describe the melanoma and its progression, which help guide the treatment plan. This system ranges from stage 0 to stage IV.12
The course of treatment for melanoma hinges on several factors, including the person’s health status, how deeply the melanoma has grown into the skin, and whether it has spread to other body parts. The team treating melanoma—which can include a dermatologist and/or an oncologist—typically creates a care plan specific to each person’s needs. That plan may include the following:20
In surgery, healthcare providers strive to remove the area that contains melanoma. Early melanomas may be treated with either of the following surgical procedures, which physicians perform in their office while the patient is awake:
Surgery may be sufficient for treating early melanoma. However, if the melanoma is more advanced, a person may require additional treatments to eliminate cancer cells. Some treatments occur following surgery, while others take place prior to surgery to make the cancerous area as small as possible. Treatment options include:
Healthcare professionals sometimes use medications to target melanoma cells that have certain genetic changes or proteins, called targeted therapies.26
Roughly half of melanoma cases arise from mutations in the BRAF gene. Melanoma cells with mutations in the BRAF gene make abnormal BRAF proteins that help them grow. Therapies that target abnormal BRAF proteins are called BRAF inhibitors. BRAF inhibitors can be helpful in cases of advanced melanoma that have BRAF mutations.26 To find out whether a BRAF inhibitor might help treat a specific patient, healthcare professionals may suggest testing for BRAF mutations.27 For those who qualify, the standard treatment consists of BRAF inhibitors given in combination with treatment targeting the related MEK protein, called MEK inhibitors.26
A small number of melanomas have mutations in the C-KIT gene. These mutations are more common in melanomas that occur on:26
For people who have advanced melanoma that started in one of these areas, doctors might test the melanoma cells for mutations in the C-KIT gene. If the melanoma has these genetic changes, therapies that target cells with these mutations might be helpful.26
While less common, some melanomas have other genetic changes that can be targeted with specific treatments. For example, targeted therapies are available for melanomas with mutations in the NRAS, ALK, ROS1, and NTRK genes.26
Healthcare professionals may turn to other treatments for melanoma, including:

An estimated 325,000 new cases of melanoma occurred worldwide in 2020. The same year, 57,000 people globally died from melanoma. Experts predict that instances of melanoma will increase by 50% from 2020 to 2040, reaching 500,000 per year. Projections estimate the number of deaths to increase by two-thirds, hitting nearly 100,000 per year.30
In most regions around the world, melanoma tends to affect more people assigned male at birth than those assigned female at birth.31 Geographically, the highest rates of cutaneous melanoma in 2020 were in Australia, New Zealand, Western Europe, North America, and Northern Europe, respectively. Melanoma is rare in Asia and Africa.32
Melanoma is a cancer of the skin. It arises in melanocytes—the type of skin cells that give skin its pigmentation, or color. In melanoma, these skin cells enter an uncontrolled growth cycle, leading to cancer.1
Melanoma symptoms typically involve the following:15
To identify possible instances of melanoma, dermatologists developed the ABCDEs of melanoma:16
Malignant melanoma is another term for melanoma, a cancer of the skin.2 This cancer occurs in melanocytes—the type of skin cells that cause skin to appear different shades and colors. In melanoma, growth of these cells spirals out of control, leading to cancer.1 All melanoma is cancer, even if the word “malignant” is not used.2
Nodular melanoma is a type of melanoma that often resembles the growth of a blood vessel, appearing as a dark brown or black dome-shaped bump. Roughly 15% of melanomas are nodular melanoma. Nodular melanoma is quick to invade nearby tissue. It can affect any surface of the body and is especially common on the torsos of people assigned male at birth.33
Early-stage melanoma, also known as Stage 0 or Stage I melanoma, tends to appear in specific ways. Stage 0 melanoma is contained in the outermost layer of skin, called the epidermis. It hasn’t reached any lymph nodes or other parts of the body. You may hear this type of melanoma called melanoma in situ.15
In stage I melanoma, the tumor is no greater than 2 millimeters thick. It may or may not have ulceration. In this case, the cancer has not spread to lymph nodes in the vicinity or other parts of the body.15
To spot potential melanoma, look for the following:15
To recognize potential melanoma, people may use the ABCDEs:16
Find Pfizer clinical trials for melanoma at PfizerClinicalTrials.com.
Explore melanoma clinical trials at ClinicalTrials.gov.
Area of Focus: Oncology
Melanoma is a focus area for Pfizer Oncology. To learn more about how we’re accelerating breakthroughs to outdo cancer, visit the Oncology page.
Find resources for those living with cancer and their caregivers at This is Living with Cancer.
Additional resources:
The information contained on this page is provided for your general information only. It is not intended as a substitute for seeking medical advice from a healthcare provider. Pfizer is not in the business of providing medical advice and does not engage in the practice of medicine. Pfizer under no circumstances recommends particular treatments for specific individuals and in all cases recommends consulting a physician or healthcare center before pursuing any course of treatment.