Let’s Protect Patients From the IRA
Congress passed the Inflation Reduction Act (IRA) with the intent of helping Americans facing the highest inflation rates in decades, but the law’s policies for medicines covered by Medicare could have negative consequences for patients.
For example, the IRA created a “pill penalty” that could discourage the development of medicines that typically come in pill or capsule form. It allows the government to start the price-setting process for pills and capsules seven years after small molecule medicines (e.g., tablets, capsules, and pills) are initially approved by the Food and Drug Administration (FDA). This time frame is roughly half of the current average time frame of 13–14 years before patents and exclusivities expire on medicines and generic competitors emerge. The significantly shorter time frame discourages innovation and risks leaving patients without the treatment options they desperately need.
Consequences of this pill penalty include:
Less access to the benefits of small molecule medicines. They’re small, but mighty: Small molecule medicines have significant therapeutic benefits for hard-to-treat diseases like cancer. They also have a unique ability to reach therapeutic targets inside the brain, which means they serve a critical role in the treatment of health conditions affecting the central nervous system, such as mental illness, stroke, epilepsy, and various neurodegenerative diseases.
In addition, because small molecule medicines come in a variety of pill forms, such as tablets or capsules, they are easier to take and patients often prefer them. Having the option of a pill form may improve adherence, potentially keeping patients healthier.
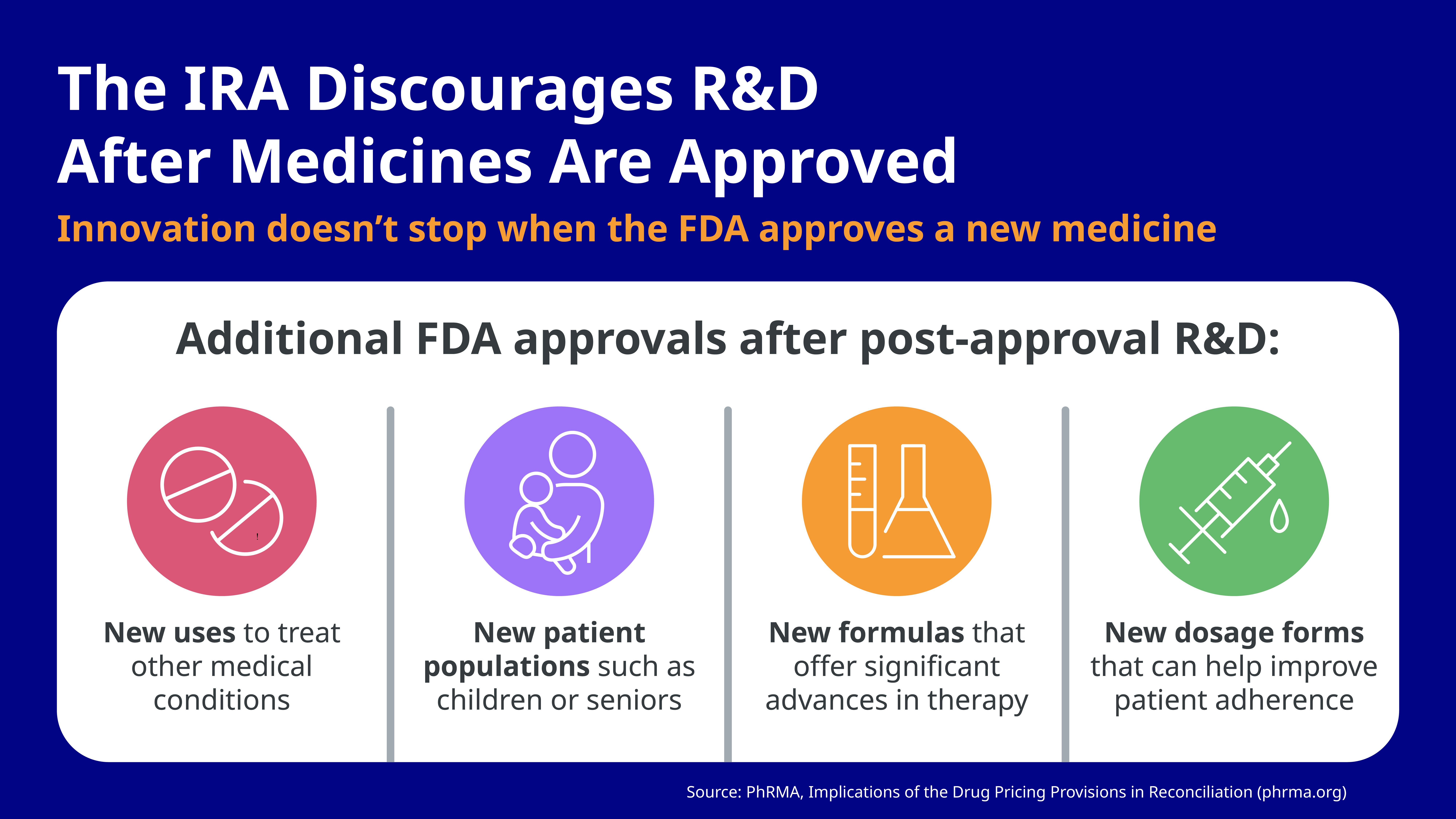
- Fewer new medicines for patients who need them. Innovation doesn’t stop when the FDA approves a new prescription medicine. Biopharmaceutical companies continue to research treatments after FDA approval, as researchers learn more and follow scientific leads after initial approval to see if these treatments can be used in new ways to improve patient care. The investments in research and development (R&D) after medicines are approved represent important advances for patients, including the development of new uses to treat a different medical condition, new patient populations such as children or seniors, new formulas, and new dosage forms.
Recent research shows how the pill penalty can discourage critical post-approval R&D — hindering innovation to fight cancer and rare diseases and disincentivizing other treatment advances. For example:
- One study of small molecule medicines approved from 2006 through 2012 found that more than half received at least one additional indication after the initial FDA approval. Of these post-approval indications, 45% were approved seven or more years after initial approval and 63% were approved five or more years after approval. 1
- Another study estimates that as many as 139 drugs over the next 10 years are at risk of not being developed because of the dangerous price-setting policies in the IRA.2
- In addition, there will be an estimated 40% reduction in new medicines being brought to market in the next 10 years.2
Less research and innovation to help treat patients with cancer. Much of the progress made in the fight against cancer is the result of research conducted on cancer medicines after the FDA first approves them. In fact, more than 60% of oncology medicines approved a decade ago received approvals for additional indications in later years, and most of those were seven or more years after initial FDA approval.3 The price-setting provisions in the IRA put this type of research on new uses for existing cancer medicines at risk.
In addition, small molecule medicines are an important part of the treatment arsenal for cancer because they can be administered orally and can enter cells to reach cancer targets. Small molecule oral-targeted therapies work by interfering with the processes that enable tumors to grow and spread throughout the body. These therapies make up the majority of cancer medicines approved. Having a broad range of both small molecule medicines and biologics is an important part of the effort to drive down cancer mortality in the years ahead.
Less research and innovation to address America’s mental health crisis. America is facing a mental health crisis, and the IRA will likely hinder the nation’s ability to overcome it. Development of new medicines to treat mental illnesses has significantly lagged behind advancements made in other areas over the past 30 years. Treatments for mental illnesses are some of the most difficult to develop — with long clinical development timelines and low success rates.
Small molecule medicines are the primary medicines used to treat patients with mental illness because they have the unique ability to reach therapeutic targets inside the brain. Despite the critical importance of these medicines to patients with mental illness, the IRA will discourage the R&D needed to bring forward new and improved treatments. For companies with R&D projects in areas such as mental health, 82% expect the IRA to have substantial impacts on their pipeline.4
- Job loss. Research estimates that the IRA’s pill penalty could result in a loss of 342,000–676,000 indirect jobs in the U.S. biopharma ecosystem.2
Additional IRA Impacts
The IRA’s pill penalty isn’t the only threat to patients. The drug pricing provision may also encourage the harmful practices of insurers and their middlemen, putting up new roadblocks for Medicare patients to access the medicines they need.
A recent analysis shows that 3.5 million Part D patients could potentially see higher out-of-pocket costs in 2026 as a direct result of the IRA’s drug pricing provisions.
Studies also show insurers have increasingly established new roadblocks to medicines for patients on Medicare, and experts predict that trend may worsen with implementation of the IRA. The IRA’s policies would not stop the harmful practices of pharmacy benefit managers (PBMs) and their middlemen that result in seniors paying more for their medicines than they do. Without PBM reform legislation, price “negotiation” policies for prescription medicines will fall short of lowering costs for patients, and insurers and their middlemen will still find ways to limit patient access to medicine.
Congress Should Prioritize Innovation and Patient Access
Congress must protect healthcare innovation and patient access to life-saving treatments. That starts with fixing the pill penalty and implementing PBM reform.
The good news is that solutions are already in the works: The bipartisan Ensuring Pathways to Innovative Cures (EPIC) ACT would help fix the pill penalty by extending the price-setting time frame for small molecule medicines to 13 years. Several PBM reform bills are also moving through Congress.
It’s time to get these bills passed to support the development of groundbreaking cures and help patients access the medicines they need!
Join Pfizer’s Ready for Cures
Stay up to date: Sign up below to join Pfizer’s Ready for Cures community to stay up to date on the IRA and learn about smart policies that can help support medical innovation and increase patients’ access to the medicines they need.
- Partnership for Health Analytic Research. “Implications of the Inflation Reduction Act price setting provisions on post-approval indications for small molecule medicines,” June 2023. https://www.pharllc.com/wp-content/uploads/2023/05/Implications-of-the-IRA-on-Post-Approval-Small-Molecules-2006-2012_Final.pdf
- Vital Transformation. “IRA’s Impact on the US biopharma ecosystem,” 2023. https://vitaltransformation.com/2023/05/iras-impact-on-the-us-biopharma-ecosystem
- Partnership for Health Analytic Research. “Implications of the Inflation Reduction Act on Post-Approval Research & Development of Biopharmaceutical Medicines,” November 9, 2022. https://www.pharllc.com/wp-content/uploads/2022/11/Clinical-Benefits-of-Post-Authorization-Research-Brief.pdf
- PhRMA. “WTAS: Inflation Reduction Act already impacting R&D decisions,” January 17, 2023.
