Early Detection is Key
In the fight against cancer, every screening, every result, every early detection matters. Join the fight against cancer and get screened at PfizerForAll.com/Screenings.
![]()
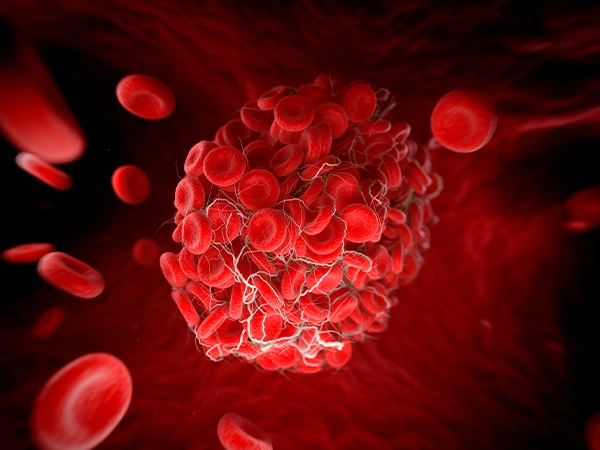
Multiple myeloma is a type of cancer that forms in certain immune system cells called plasma cells. Healthy plasma cells are in bone marrow, the inner portion of some bones throughout the body.1
In healthy individuals, infections trigger B cells, a type of white blood cell, to mature into plasma cells to fight the infection. Then, plasma cells make specific proteins, called antibodies or immunoglobulins, which identify and destroy foreign substances or invasive microbes that may cause disease.1,2,3
B cells can also transform into cancerous plasma cells that divide out of control and produce abnormal antibodies called M proteins.4 This type of cancer, known as multiple myeloma, may cause additional complications that affect the bones, blood, and other organs which, in turn, may lead to additional health issues.2
There are other types of plasma cell disorders that don’t meet the diagnostic criteria for multiple myeloma. Some of these conditions act more like precursors for multiple myeloma. They include monoclonal gammopathy of uncertain significance (MGUS) and smoldering multiple myeloma (SMM).1
In the United States, a person’s risk of developing multiple myeloma in their lifetime is less than 1 percent. According to the American Cancer Society, about 36,000 new cases of multiple myeloma will be diagnosed in the U.S. in 2025.5
This type of cancer is much more common among older adults at least 65 years old: The average age at diagnosis is 69 years old.5 People 45 years old and younger rarely develop the disease. Certain factors make a person more likely to develop myeloma, including being assigned male at birth or being Black.2
There is currently no known cure for multiple myeloma, but the mortality rate, or the number of deaths resulting from the disease, has consistently declined since the mid 1990s.6,7 Survival rates are expected to continue to improve thanks to the many new treatments for multiple myeloma approved in recent years. There are also more treatments currently in development that may help further boost survival rates.7

The exact causes of multiple myeloma are unknown. However, scientists do understand that all cancers result from changes to cellular DNA. Inside cells, DNA comes together to form genes that direct various functions, like cellular growth, division, and repair.8 Although scientists have identified some of the gene mutations that may cause multiple myeloma, the causes of such mutations aren’t clear. Some people may inherit genetic mutations from their parents. On the other hand, certain genetic mutations may just occur over a person’s lifetime independently or because of outside factors, like exposure to radiation. In some cases, the genetic mutations that occur in multiple myeloma cells seem to occur for no reason at all.8
Multiple myeloma may run in some families, but the disease is usually not thought to be hereditary.9,10,11 In other words, several family members can all have multiple myeloma. However, research suggests the mutations causing multiple myeloma do not pass down through family members.9 While family history is a risk factor, most people who develop multiple myeloma do not have a family history of the disease.11
As with any type of cancer, certain risk factors may raise a person’s likelihood of developing multiple myeloma. However, having one or several risk factors still isn’t a guarantee that cancer will develop.11
The risk of multiple myeloma increases as a person gets older. Doctors diagnose most cases in people over age 65.11
People who are assigned male at birth are slightly more likely to develop multiple myeloma compared to those assigned female at birth.11
Research suggests that Black people are more than twice as likely to develop multiple myeloma compared to people who are White. The reason for this difference is unknown.11
A personal history of other plasma cell diseases, such as MGUS or solitary plasmacytoma, may put you at higher risk for multiple myeloma.11
Exposure to radiation, certain chemicals like Agent Orange, and some metals like cadmium or lead may be linked to multiple myeloma.11,12
Being overweight or obese raises the risk of developing multiple myeloma.11
Currently, there is no known way to prevent multiple myeloma. However, you can help lower your risk by avoiding chemicals and radiation that may increase your risk. Losing weight and maintaining a healthy weight may also help.13
There are several different types of active multiple myeloma, which are identified by the type of antibody (immunoglobulin) that’s overproduced by cancerous plasma cells. In some cases, a precancerous condition known as smoldering multiple myeloma (SMM) develops into active multiple myeloma over time.14
Generally, people diagnosed with SMM have no symptoms. Instead, doctors often discover the condition by chance while testing or treating a person for another issue. Many people with SMM don’t need treatment initially, but regular monitoring may be necessary to ensure the condition doesn’t develop into active multiple myeloma. If a person has SMM, they have a 50 percent risk of developing myeloma within five years and a 65 percent risk of developing myeloma within 10 years.14
There are five different types of active multiple myeloma. Each is characterized by an overproduction of different antibodies:14
Other types of myelomas include light-chain myeloma and nonsecretory myeloma.14
Light-chain myeloma makes up about 15 percent of all cases, making it the third most common type of myeloma following IgG and IgA myelomas. In this type of myeloma, cancerous plasma cells produce incomplete antibodies (immunoglobulins)—the only portion produced is known as the “light chain”.14
This rare form of myeloma makes up 3-5 percent of diagnoses. Unlike other types of myelomas, nonsecretory myeloma cells don’t make or release any excess antibodies. Because of this, nonsecretory myeloma may be harder to detect with standard blood or urine tests.14
There are several conditions related to active multiple myeloma, some of which are not cancerous:14
The symptoms of multiple myeloma may vary greatly from person to person. Some people experience no symptoms in the early stages of the disease. Others experience symptoms only detectable by healthcare professionals during examination.16
The most common symptoms of multiple myeloma include:16
It’s possible to experience other symptoms as well, including:16
Multiple myeloma is a serious disease that may cause complications because of the overproduction of plasma cells and M protein. These complications might include:16,17
If you have any signs or symptoms of multiple myeloma, your doctor may recommend further testing. These tests may include blood tests, urine tests, biopsies, or imaging tests.18
Doctors sometimes use an acronym, CRAB, to label signs of myeloma:17
Doctors use CRAB to help determine whether a person has active multiple myeloma. If a person shows one or more CRAB signs, and at least 10 percent of their bone marrow contains cancerous plasma cells, doctors typically diagnose active myeloma and begin treatment.17
Doctors may also use other test results to diagnose myeloma such as a high number of plasma cells in the bone marrow, more than one myeloma lesion found via body scan (MRI) and abnormal levels of M-proteins.18,19
Laboratory testing helps your doctor make an accurate diagnosis, track disease progression, and determine how well recommended treatments are working.19
Various laboratory tests your doctor may suggest include:
Biopsies may also be used to help your doctor diagnose multiple myeloma. During a biopsy, a healthcare professional removes a small sample of tissue for further testing in a lab.19
Many people undergo a bone marrow aspiration or biopsy to look for abnormal plasma cells. This takes place at your doctor’s office or at a hospital.19,20 Samples are typically collected from the back of the hip (pelvic) bone but may be taken from elsewhere if appropriate. The biopsy may remove a small portion of a bone that includes the marrow.19 Or, a healthcare professional may collect a liquid bone marrow sample (aspiration).19,20
If you have a bone marrow aspiration, the sample may also be used for other tests to:
Needle biopsies help doctors learn more about suspected plasma cell tumors (plasmacytomas) that occur in the soft tissues of the body. Healthcare professionals typically use two different types of needle biopsies:19
Imaging tests are an important part of the diagnostic process. They may be recommended for several reasons, including identifying areas of the body where cancer might be present, seeing if the cancer has spread, and determining whether treatment is effective. Imaging tests your doctor may recommend include:19,20
Treating multiple myeloma takes a team effort, and several therapies are available, depending on each person’s unique needs. Doctors usually recommend local or systemic therapies, sometimes suggesting a combination of the two. Your care team will check you closely at regular intervals, depending on the type of myeloma diagnosed and your treatment plan.21
These options target only one specific portion of the body. Typically, doctors use local treatments when multiple myeloma isn’t too advanced.21
Although it’s not a common treatment, doctors sometimes use surgery to remove singular plasma cell tumors (plasmacytomas) from the body. In some cases, emergency surgery is necessary to help manage complications from multiple myeloma, such as spinal cord compression. Doctors may also recommend surgery to attach plates or rods to weakened bones to help support them and treat or prevent breaks.22
Radiation uses high-energy particles that target and kill cancer cells. In cases of multiple myeloma, radiation might be used when other treatments, like medications, have not worked. Radiation is also typically used to treat isolated plasmacytomas.23
In most cases, external beam radiation therapy helps treat multiple myeloma. With this type of therapy, a machine outside the body delivers radiation directly to affected tissues. The number of radiation treatments varies depending on each person’s needs.23
Systemic therapies affect cancer cells throughout the entire body.21 This is usually the main way doctors treat multiple myeloma, and most treatment plans use two to four different kinds of drugs for greater effectiveness. However, your treatment plan depends on your age, overall health, kidney function, the type of myeloma you have, and whether a stem cell transplant is part of your treatment plan.24
Common drug treatments for multiple myeloma include:24
In some cases, doctors use traditional chemotherapy (chemo) medications to treat multiple myeloma, although the use of chemo now occurs less frequently. Chemo medications either control the growth of cancer cells or kill them outright—they are taken either as a pill or via injection in a muscle or directly into the blood stream through an IV. If used, doctors often combine chemo medications with other treatment options. However, if a patient has a bone marrow transplant, doctors may avoid certain chemotherapy agents that can damage bone marrow.24
Doctors often recommend a stem cell transplant to treat multiple myeloma, especially if the person is younger and otherwise healthy. Individuals typically receive high-dose chemotherapy medications to first kill myeloma cells in the bone marrow. Then, the patient receives new, healthy blood-forming stem cells through an IV infusion. A stem cell transplant may be either:27
Chimeric antigen receptor (CAR) T-cell therapy helps the body’s own immune system identify and destroy cancer cells by changing genes inside some immune system cells. This enables those immune cells to better attack cancerous cells.29
During the initial procedure, called leukapheresis, healthcare professionals use an IV to remove blood and then isolate certain immune cells, called T cells, from the blood. Those T-cells go to a laboratory where they are genetically altered—this alteration helps the cells attach to specific proteins on the surface of cancer cells. After making a large batch of altered T-cells, which usually takes a few weeks, doctors infuse them back into the body. There, the altered T-cells boost the immune system, helping it destroy cancer cells.29
Also known as palliative care, supportive treatments help relieve or prevent symptoms associated with multiple myeloma. The goal of such treatments is to improve quality of life and patient comfort, regardless of any treatment goals or the cancer’s stage.30
Supportive therapies generally aim to prevent or treat infections, bone problems, low red blood cell counts, and hyperviscosity (thickening of the blood). These treatments do not address the cancer itself.30
The treatment for multiple myeloma can cause its own complications, such as:17,31

Multiple myeloma affects people worldwide. There were an estimated 188,000 cases diagnosed around the world in 2022. Researchers estimate that there were 121,000 deaths from multiple myeloma that same year.34
Multiple myeloma most often occurs in North America (19 percent of global cases) or Eastern Asia (21 percent of global cases). The incidence rate of the disease, or the number of new cases among a group of people over time, is highest in North America and in Australia/New Zealand. However, mortality rates, or how many people actually die from the disease, were highest in Australia/New Zealand, Northern Europe, and South Africa.34
Researchers estimate that, if rates of multiple myeloma diagnosis and death remain unchanged, estimated case numbers will increase by 71 percent worldwide by 2045, relative to 2022. Additionally, the number of deaths due to multiple myeloma is projected to increase by 79 percent in the same time frame.34
Fortunately, there are a range of treatment options available for people diagnosed with multiple myeloma.21,24 If myeloma is found early or if you have a precancerous condition like smoldering multiple myeloma and you don’t have symptoms, immediate treatment might not be necessary.14,35
Your cancer care team will put together a treatment plan based on your personal needs.22 Your options may include chemotherapy, radiation therapy, stem cell transplant, other medications, or supportive therapy.35 Treatment often consists of several different therapies combined.21
There is currently no recommended screening test for multiple myeloma.36 If your doctor suspects multiple myeloma, they may recommend further testing to help arrive at a diagnosis. These tests may include laboratory tests, biopsies, or imaging tests.19
Many people do not experience symptoms when multiple myeloma is in its early stages. If symptoms are present, they may be extremely hard to detect except by a healthcare professional.16
Some of the more common symptoms of multiple myeloma include fatigue, bone problems, kidney problems, low blood counts, and frequent infections.16
While there is currently no cure for multiple myeloma, several new treatments have been approved in recent years, and others are in development. With treatment, many people experience a remission in the disease and its symptoms. This may go on for several years before any relapse.6,7
Multiple myeloma is not thought of as a hereditary disease because no specific inherited genetic factors have been identified.9 However, there are instances where members of the same family develop multiple myeloma.10,11
Even though doctors don’t know the exact cause of multiple myeloma, researchers do link the disease to DNA changes in plasma cells.2,8 These DNA changes either promote the activity of oncogenes, a mutated gene that may cause cancer, or they prevent the action of tumor suppressor genes, which help manage cellular growth and division.37
Find a Pfizer trial for multiple myeloma at PfizerClinicalTrials.com
Explore multiple myeloma clinical trials at ClinicalTrials.gov
Area of Focus: Oncology
Multiple Myeloma is a focus area for Pfizer Oncology. To learn more about how we’re accelerating breakthroughs to outdo cancer, visit the Oncology page.
Find resources for those living with cancer and their caregivers at This is Living with Cancer.
Learn more about Pfizer’s commitment to people living with blood cancer.
The information contained on this page is provided for your general information only. It is not intended as a substitute for seeking medical advice from a healthcare provider. Pfizer is not in the business of providing medical advice and does not engage in the practice of medicine. Pfizer under no circumstances recommends particular treatments for specific individuals and in all cases recommends consulting a physician or healthcare center before pursuing any course of treatment.