Lung Cancer: The Facts
If someone were to ask you what the leading cause of cancer-related death is in the US, you might guess colon cancer, breast cancer, or prostate cancer. The correct answer is actually lung cancer. It’s also the second most diagnosed cancer in the US in both men and women. Most people diagnosed with lung cancer are 65 or older. However, it can occur in younger people, too. It may also surprise you to know that up to 20% of people who die from lung cancer in the US have never smoked or used tobacco products.
It’s important to speak with your healthcare provider about any questions or concerns you may have about lung cancer, how it can be prevented, what screening tests are available, and which treatments might be right for you. Read on to learn more.
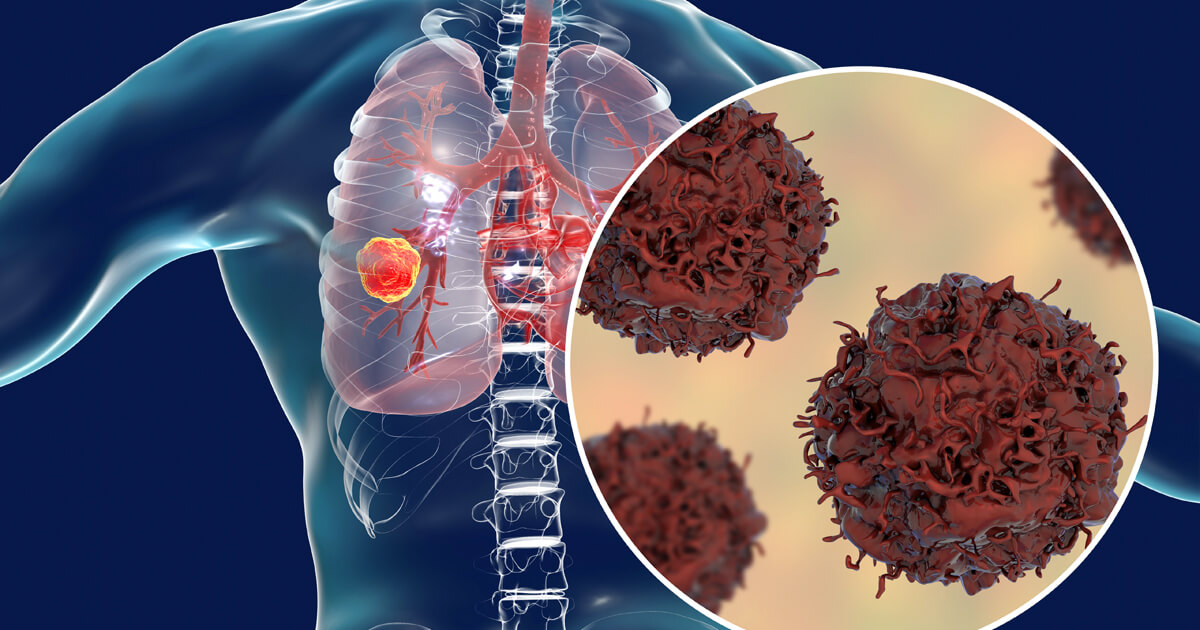
What is lung cancer?
In general, cancer happens when cells in the body grow out of control. In this case, it starts in the lungs, and is therefore called lung cancer. But when cancer cells from the lungs travel to other parts of the body, such as the lymph nodes or brain, these are called metastases.
There are 2 major types of lung cancer:
- Small cell. This type accounts for 15% of all lung cancers and is more aggressive than non-small cell lung cancer.
- Non-small cell.This is the most common type and accounts for 85% of all lung cancers. There are 3 major subtypes of non-small cell lung cancer, which include adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Other types of lung cancer include mesothelioma and lung carcinoid.

What are the causes and risks factors?
Several risk factors can increase your chances of developing lung cancer. Keep in mind that having a risk factor doesn’t mean you’ll get lung cancer.
Risk factors for lung cancer include:
- Smoking. About 80% of lung cancer deaths are thought to be caused by smoking. The risk for developing lung cancer increases the longer and more often a person smokes. Lung cancer can occur even in people who have never smoked.
- Secondhand smoke. More than 7,000 people die each year from lung cancer due to secondhand smoke.
- Exposure to radon, asbestos, air pollution, and cancer-causing agents in the workplace.
- Previous radiation therapy to the lungs for other cancers.
- Personal or family history of lung cancer.
In some people, having one or more of these risk factors can lead to genetic mutations in certain genes. These mutations can cause cells to divide and grow out of control, forming cancerous tumors. Some common lung cancer mutations involve the TP53, EGFR, and KRAS genes.
What are the signs and symptoms?
Each person may have different signs and symptoms. Most people may not even have any symptoms until their lung cancer is very advanced or their tumor has grown.
Lung cancer symptoms may include:
- A cough that doesn’t go away or gets worse, with or without blood.
- Chest pain.
- Shortness of breath.
- Wheezing.
- Repeatedly having pneumonia or bronchitis.
- Feeling tired more than normal.
- Weight loss for no reason.
- Loss of appetite.
If you experience any of these symptoms, talk with your healthcare provider.
How is lung cancer diagnosed?
If your healthcare provider suspects you might have lung cancer, he or she may perform a physical exam and order certain tests. These tests may include:
- Chest x-ray. This is often the first test your healthcare provider will do.
- CT scan. This scan rotates around your body and takes pictures. CT scans are more likely to show lung tumors than a chest x-ray.
- Sputum cytology. This test studies your mucus that you cough up (sputum) under a microscope in search of cancer cells.
- PET scan. This exam scans your brain and other parts of the body to see if the cancer spread.
Only a biopsy can confirm a lung cancer diagnosis. A biopsy is done by taking a small tissue sample from the lungs and studying it under a microscope to see if it has cancer cells. Once a diagnosis is made, other tests are run to find out if and how far the cancer has spread through the lungs, lymph nodes, and the rest of the body. This process is called staging. The stage of the cancer describes the size of the cancer, where it is and, whether it has spread. Knowing the type and stage of lung cancer helps your healthcare provider determine which treatments to use.
For people who are at high risk for developing lung cancer, screenings are recommended because they can help detect cancer early. If you have a history of heavy smoking, are currently smoking, have quit smoking within the past 15 years, and are between the ages of 55 and 80, you should speak with your healthcare provider about getting screened.
What treatments are available?
Treating lung cancer depends on which type it is, how far it has spread, and which biomarkers are found during biomarker testing. Biomarkers tell you what is inside the lung cancer cells that might be driving the tumor’s growth. Once those factors are determined, your healthcare provider can understand more about the tumor and recommend which therapies might work the best for you. Available treatments include:
- Chemotherapy.
- Radiation.
- Targeted therapy.
- Immunotherapy.
- Surgery.
- A combination of these treatments.
Talking with your healthcare provider about any questions you may have about cancer is an important part of staying informed about your health. Download this discussion guide to help you have a more meaningful discussion with your healthcare team.
[1][2][3][4][5][6][7][8][9][10][11]
References
- 1. American Cancer Society. Lung Cancer Risk Factors. Accessed September 10, 2018.
- 2. American Cancer Society. Key Statistics for Lung Cancer. Accessed August 29, 2018.
- 3. American Cancer Society. Lung Cancer Risks for Non-smokers. Accessed September 10, 2018.
- 4. Centers for Disease Control and Prevention. What Is Lung Cancer? Accessed September 10, 2018.
- 5. OncoLink. Lung Cancer: The Basics. Accessed August 29, 2018.
- 6. Genetics Home Reference. Lung Cancer. Accessed October 8, 2018.
- 7. Centers for Disease Control and Prevention. What Are the Symptoms of Lung Cancer? Accessed August 29, 2018.
- 8. American Cancer Society. Exams and Tests That Look for Lung Cancer. Accessed August 29, 2018.
- 9. Centers for Disease Control and Prevention. How Is Lung Cancer Diagnosed and Treated? Accessed August 29, 2018.
- 10. Centers for Disease Control and Prevention. Who Should Be Screened for Lung Cancer? Accessed August 29, 2018.
- 11. Lungcancer.org. Lung Cancer: New Tools for Making Decisions About Treatment. Accessed September 10, 2018.
